What is Extravasation, Infiltration, and Phlebitis?
Extravasation, Infiltration, and Phlebitis are most common local complications of the peripheral intravenous (IV) therapy. There are similarities and significant differences between each of those conditions.
According to the research evidence, 58.7% to 86.7% of patients have a peripheral venous catheter (PVC) inserted during their hospitalization. Generally, nurses are responsible for insertion, management, and care of PVCs of hospitalized patients.
Therefore, as nurses, we should be familiar with similarities and differences of extravasation, infiltration, and phlebitis. Because it will help us to take appropriate nursing interventions earlier in case of such complications.
Here, we’ll discuss
- definition,
- causes,
- signs and symptoms,
- nursing intervention and management, and
- prevention of extravasation, infiltration, and phlebitis.
Extravasation
Definition of Extravasation
Medically Extravasation is referred to a condition where blood, serum, lymph or infusion leaks into the surrounding tissues.
Here we’ll discuss specially about extravasation caused by IV therapy.
Extravasation in IV therapy can be described as leakage of vesicant IV solutions or medications into the surrounding tissues or skin of the catheter site.
Vesicants are IV solutions and medications that have pH less than 5 or greater than 9, highly concentrated (i.e: osmolarity above 600 mOsm/L), or vasoconstrictive (cause the blood vessels to constrict).
Most of the chemotherapy drugs are vesicants. Some of the examples of non-chemo vesicant drugs include:
- Phenergan (promethazine)
- Vancomycin
- IV contrast
- Vasopressors
Extravasation can cause pain, inflammation, blistering of the local skin and underlying structures. And, if left untreated, it may even result in permanent tissue damage and necrosis.
What are the causes of Extravasation?
- Puncturing of the opposite or same vein during insertion
- Improper placement
- Dislodged cannula /catheter
- Occlusion of the vein causing backflow of blood
- Inflammatory process that causes fluid leak at capillary level
- Erosion of the vessel by the catheter
Risk factors of Extravasation
- Multiple manipulations of infusion delivery system
- Large gauge and length of catheter
- Failure to stabilize VAD (vascular access device) properly
- Patient age, condition, acuity
- Administration of irritating drugs and/or solutions via a peripheral VAD
- Poor VAD insertion technique
- Inappropriate care and maintenance practices
- Prolonged dwell time
Signs and symptoms of Extravasation
- Local pain and swelling
- Blanching, tight skin, burning
- Changes in skin color
- Cool skin around the I.V. site
- Blistering and sloughing, or necrosis
- Fluid leakage from insertion site
- Slow capillary refill
- Numbness, tingling, paresthesia
- Deep pitting edema and circulatory impairment
- If untreated: necrosis
Treatment of Extravasation
The treatment of extravasation depends on various contributing factors, such as
- type of the drug involved
- volume the fluid leaked into the surrounding area
- extravasation site
The early initiation of treatment is critical in the management of extravasation to prevent tissue damage and necrosis.
Nursing interventions and management of Extravasation
- Stop infusion immediately
- Aspirate for infused medication with a small syringe before removal
- Notify the prescriber and implement extravasation protocol as per advice
- Elevate the extremity
- Obtain new vascular access from the opposite side
- Perform frequent assessments of sensation, motor function, and circulation of the affected extremity
- Administer the appropriate antidote according to the facility’s protocol. For example:
- Sodium thiosulfate for alkylating agents
- Dexrazoxane for anthracyclines
- Hyaluronidase for plant alkaloids
- Phentolamine for vasopressors (e.g., dopamine, epinephrine, metaraminol)
- Apply thermal therapy – warm and cold compression for extraversion depends on the type of vesicant. For example:
- Cold compression is recommended for alkylating agents, anthracyclines, antitumor antibodies, and taxanes.
- Heat is recommended for plant alkaloids, vasoconstricting agents (e.g. dopamine, dobutamine, epinephrine)
- Observe site for signs and symptoms of compartment syndrome, nerve injury, blisters, skin sloughing, tissue necrosis, and functional and sensory loss
- Monitor the site at 24hr, 1 week, 2 week, and as needed. Also, INS suggests taking pictures of the site during these assessments.
- For all central venous catheters, obtain a study to identify the cause of the problem
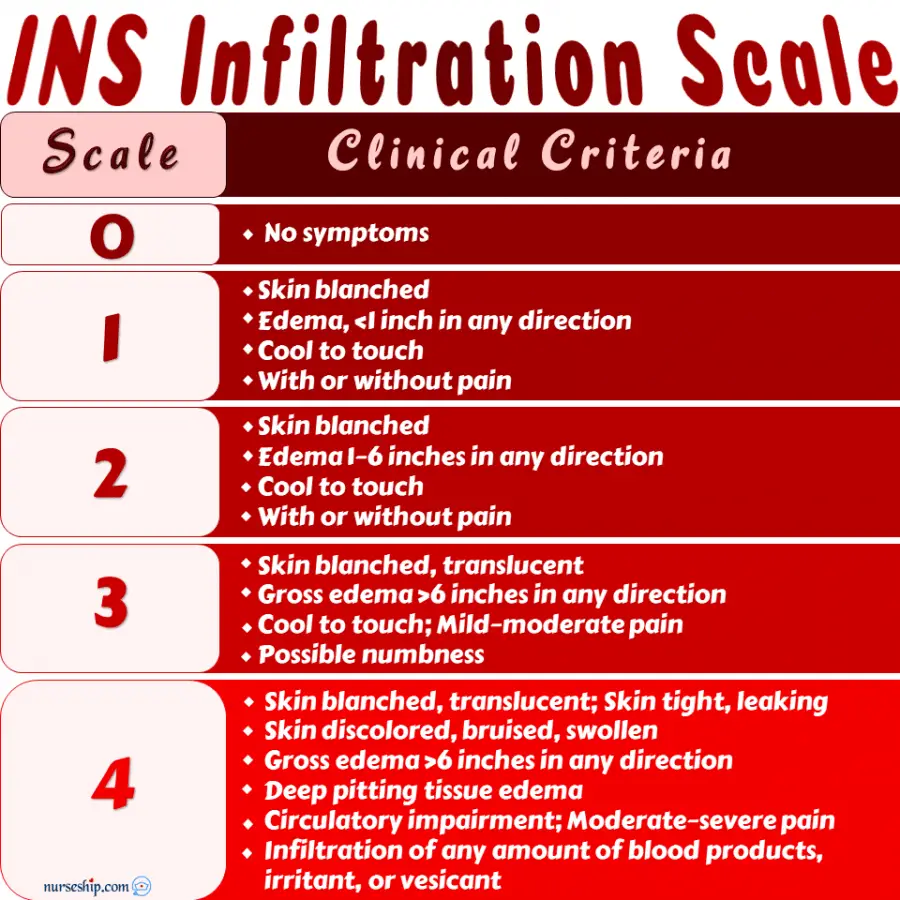
- Rate the extravasation site using a standardized grading scale (eg: INS Infiltration Scale) and document the incident
Prevention of Extravasation
Preventive measures for extraversion include:
- Use smallest size catheter to give the infusion
- Consider and collaborate with doctor for CVAD to administer drugs and infusion with a pH less than 5 or greater than 9, or osmolarity greater than 600 mOsm/L, or final dextrose concentration greater than 10%
- Avoid inserting IV catheters near joint flexion and the lower extremities
- Avoid veins in the digits, hands, and wrist because of the close network of tendons and nerves
- Avoid re-cannulation close to previous sites
- Proper stabilize catheter to prevent movement at the insertion site
- Ensure adequate patency of VAD before starting the infusion
- Instruct patient to immediately report any pain, burning, or swelling with infusion administration
- Strictly adhere to proper administration techniques
Infiltration
Definition of Infiltration
IV Infiltration can be defined as the process in which non-vesicant fluids leaks into the surrounding tissues of the IV site.
Usually, infiltration is less harmful because it occurs as result of leakage of non-vesicant (i.e: iv solutions and medications that doesn’t irritate surrounding tissue).
IV infiltration and extravasation involve the same process, they differ only by the type of fluid leaks into the extravascular space.
When non-vesicant fluid leaks to the surrounding tissue is known as IV infiltration. Similarly, when vesicant fluid leaks to the surrounding tissue is known as IV extravasation.
So, the causes and risk factors for IV infiltration is same as extravasation.
Signs and symptoms of Infiltration
- No free flow of IV fluid
- Local swelling, discomfort, and pain
- Blanching, tight skin, burning
- Cold and discolored skin around the I.V. site
- Fluid leakage from insertion site
Nursing intervention and management of Infiltration
- Stop the infusion immediately
- Aspirate fluid from catheter with a small syringe and remove catheter
- Apply sterile dressing if there is oozing from site
- Apply thermal therapy according to facility’s protocol
- Warm compress helps to increase circulation to the area and speed up the healing process
- Cold compress may be used reduce swelling and discomfort
- Elevate the extremity
- Obtain a new IV access in the opposite extremity
- Rate the infiltration using standardized grading scale (eg: INS Infiltration Scale) and document the incident
Prevention of Infiltration
- Select appropriate size catheter and vein.
- Avoid areas of flexion, veins in extremities with preexisting edema, or veins in areas with known neurologic impairment.
- Monitor the I.V. site frequently for any sign or symptoms.
- Ensure competency of venipuncture skill and techniques
- Strictly adhere to proper administration techniques.
Documentation Tips for Extravasation and Infiltration
- Patient’s details
- Date and time of extravasation or infiltration
- Catheter size and type
- Whether the extravasation/infiltration location is new or a preexisting site
- Name of the drug administered, method of administration, and estimated volume of fluid infiltration
- Patient complaints and signs and symptoms of extravasation/infiltration
- Appearance of the site
- Implemented nursing interventions and its outcome
- Event reporting as per facility’s policy
INS Infiltration Scale
Phlebitis
Definition of Phlebitis
Phlebitis is also known as Venitis is an inflammation of the vein. Trauma during insertion, movement of the PVCs and certain drugs and infusions can irritate the vein and cause inflammation.
Phlebitis can become dangerous and life-threatening in cases of blood clot formation. This condition in called Thrombophlebitis.
Although there are several other conditions that may lead to phlebitis and thrombophlebitis. Here, we’ll discuss phlebitis in relation to IV therapy.
Click here to see a list of NANDA Nursing Diagnosis for Thrombophlebitis.
Types of Phlebitis
There are four types of phlebitis. Namely, Mechanical Phlebitis, Chemical Phlebitis, Bacterial Phlebitis, and Post-Infusion Phlebitis.
Mechanical Phlebitis
Mechanical phlebitis occurs when movement of the catheter inside the vein causes friction and inflammation. Also, if the catheter size is simply too big for the vein.
Causes for Mechanical Phlebitis
Causes for mechanical phlebitis include:
- Unsuitable site selection such as using areas of flexion
- Large catheter size
- Poorly secured catheter
- Injury during insertion
Chemical Phlebitis
Chemical phlebitis occurs as a response to certain drugs and/or fluids infused through the catheter.
Causes for Chemical Phlebitis
Causes for chemical phlebitisinclude:
- Irritating drugs and solutions
- Improperly diluted drugs and infusions.
- Rapid administration of drugs and IV fluids
- Catheter material
- Prolonged use of same catheter
Bacterial Phlebitis
Bacterial phlebitis is inflammation of the vein wall caused by bacterial infection.
This can create serious complications due to the potential for the development of bloodstream infection that can result in systemic sepsis.
Causes for Bacterial Phlebitis
Causes for bacterial phlebitis include:
- Improper hand hygiene
- Poor aseptic precaution during insertion or infusion
- Poor catheter insertion techniques
- Improperly fixed catheters
- Prolonged use of same catheter
- Failure to assess and identify early signs of phlebitis
Post-infusion phlebitis
Post-infusion phlebitis is inflammation of the vein that shows up 48 to 96 hours after removal of the catheter.
Incidences of post-infusion phlebitis is usually related to the catheter material and extended dwell time of the catheter in the patient’s vein.
Causes for Post-Infusion Phlebitis
Causes for post-infusion phlebitis include:
- Catheter material
- Poor catheter insertion technique
- Prolonged use of same catheter
- Fragile patients
- Poor vein condition
- Hypertonic or acidic solutions
- Ineffective filtration
- Big catheter size for the vein
- Poor VAD care and maintenance practices
Risk factors of phlebitis
- Acidic or hypertonic IV solutions
- Rapid IV rate
- Administration of IV drugs such as KCl, Vancomycin, and Penicillin
- Inserting VAD close to areas of flexion
- Poorly fixed catheters
- Improper hand hygiene
- Lack of aseptic technique
Signs and symptoms of Phlebitis
- Pain
- Erythema
- Swelling
- Vein may become hard and cord-like
Nursing intervention and management of Phlebitis
- Remove catheter immediately with first sign of phlebitis
- Determine the cause of phlebitis
- Assess the catheter site frequently
- Notify the prescriber the degree of phlebitis
- Apply warm compress for 20 minutes, 3 to 4 times per day as per advice
- Secure a new IV access in the opposite extremity
- Document the incident
Prevention of Phlebitis
Preventive measures of phlebitis are:
- Choose smallest size and shortest length catheter for the required IV therapy
- Avoid inserting catheter too close to joints of flexion
- Avoid infusing irritant drugs or solution (i.e: fluids with pH less than 5 or more than 9, osmolarity above 600 mOsm/L, and dextrose concentration above 10%) via peripheral lines.
- Adhere to strict aseptic measures during catheter insertion and giving medication
- Properly stabilize VAD to prevent moving of the catheter
- The INS Standards of Practice (2011) recommends to change peripheral IV catheter only if clinically indicated in adults. And also, to avoid routine change of peripheral IV catheters in infants and children.
Documentation Tips for Phlebitis
When documenting the incidences of phlebitis include:
- Patient’s details
- Date and time of the phlebitis
- Severity of the phlebitis according to standardized phlebitis grading scale
- Drug or solution being infused
- Size and dwell time of the catheter
- Nursing interventions implemented for phlebitis
- Outcome of the intervention
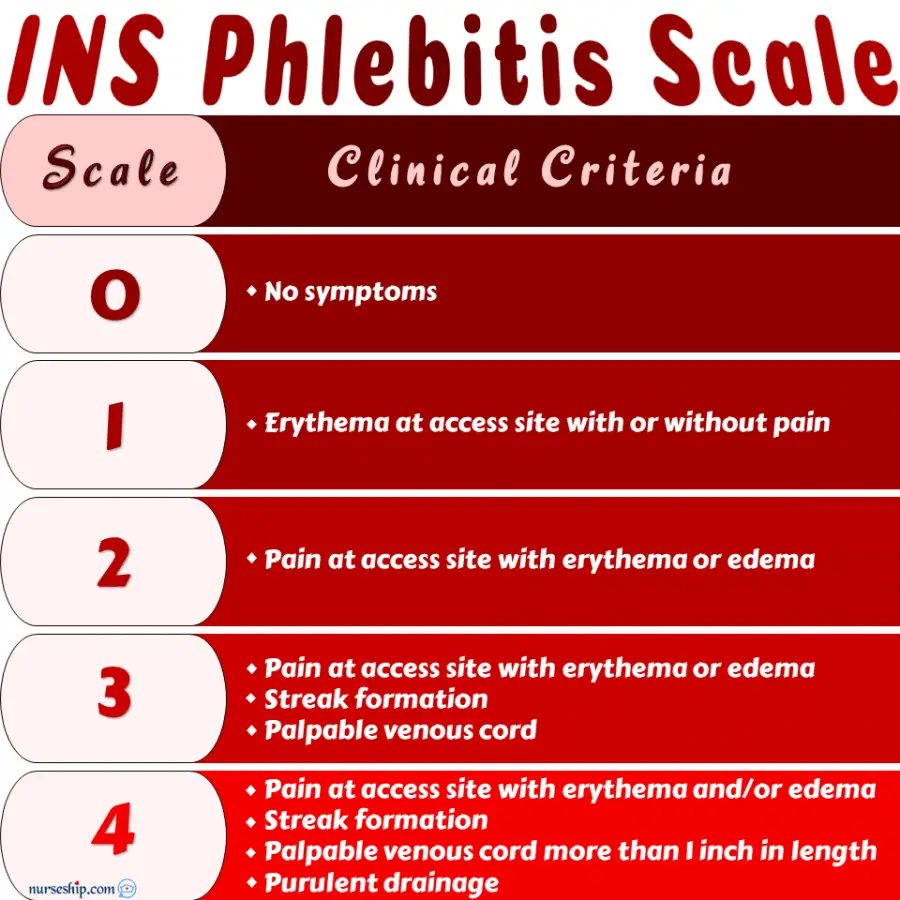
INS Phlebitis Scale
Click here to see a list of NANDA Nursing Diagnosis for Thrombophlebitis.
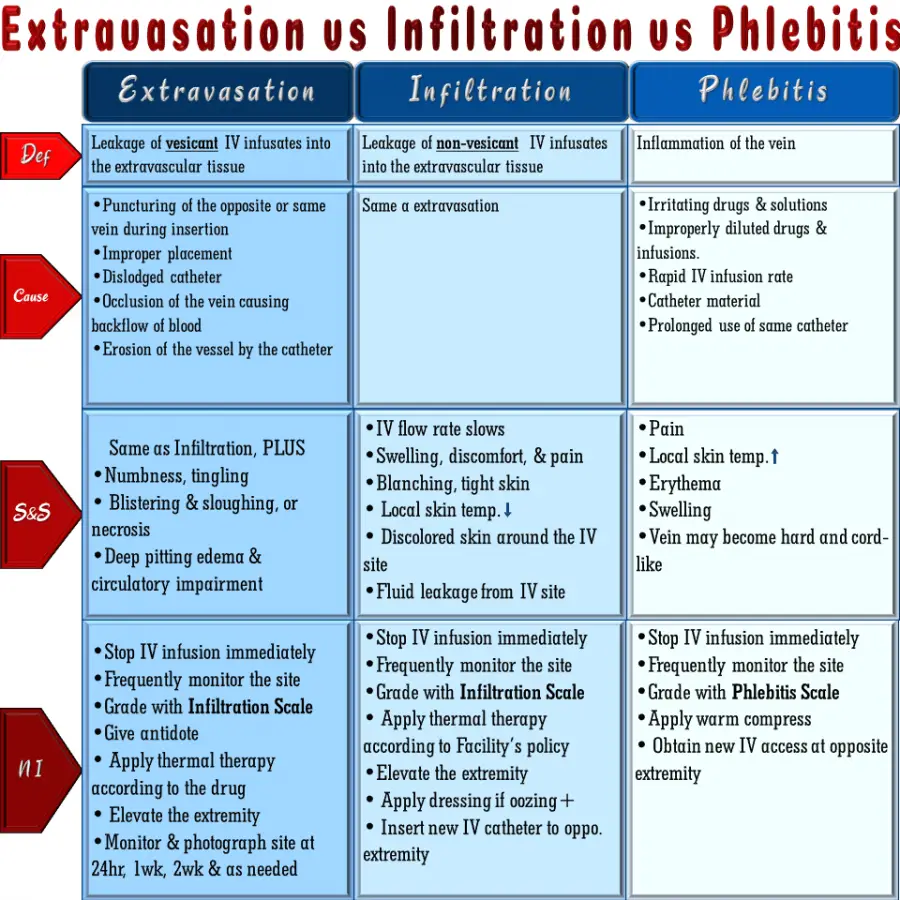
Extravasation vs Infiltration vs Phlebitis
The following table is comparison of extravasation, infiltration, and phlebitis.
Reference
Alexander, M., Corrigan, A., Gorski, L., & Phillips, L. (2014). Core Curriculum for Infusion Nursing (4th ed.). Wolters Kluwer Health | Lippincott Williams & Wilkins.
Ignatavicius, D., Workman, M., Blair, M., Rebar, C., & Winkelman, C. (2016). Medical-Surgical Nursing: Patient-Centered Collaborative Care (8th ed.). Elsevier.
O’Toole, M. (2013). MOSBY’S MEDICAL DICTIONARY (9th ed.). Elsevier.
Potter, P., Perry, A., Stockert, P., & Hall, A. (2013). Fundamentals of Nursing (8th ed.). Mosby, Elsevier Inc.
Toland, S. (2017). Guidelines for the Management of Extravasation of a Systemic Anti-Cancer Therapy including Cytotoxic Agents [Ebook]. Retrieved from https://www.england.nhs.uk/midlands/wp-content/uploads/sites/46/2019/05/management-extravasation-of-a-systemic-anti-cancer-therapy-including-cytotoxic-agents.pdf