Last updated on December 28th, 2023
In this article, you will learn about what is fetal heart rate monitoring and VEAL CHOP MINE in nursing.
Related Article: What is Baseline Fetal Heart Rate (FHR)?
What is fetal heart rate monitoring?
Fetal heart rate (FHR) monitoring can be defined as the close observation of fetal behavior during the delivery.
Fetal heart rate assessment is the key tool for monitoring the status of the fetus during labor. It gives an indirect indication of the oxygen status of the fetus.
FHR monitoring is crucial during labor because of the frequent changes in intrauterine pressure with the contractions.
Additionally, even in normal deliveries fetus experiences distress due to:
- Uterine contraction reduces uteroplacental circulation
- Uterine contraction affects intrauterine pressure
- Head compression affects the function of the vital brain centers
What is the goal of fetal heart monitoring during labor?
The goal of fetal heart rate monitoring during labor is:
- to identify the well-being of the fetus
- to identify signs of fetal compromises, such as fetal hypoxia
- to implement interventions as soon as possible to ensure the safe delivery of the baby
Severe hypoxia in labor along with metabolic acidosis can cause fetal organ damage or fetal death. Therefore, as nurses, we must know what to look for and when to take action.
What are the methods of fetal heart rate monitoring?
The fetal heart rate can be monitored either (1) intermittently or (2) continuously with an electronic device.
1. Intermittent auscultation
Intermittent fetal heart rate monitoring involves periodic auscultation of FHR using an ordinary stethoscope, or a fetoscope, or a hand-held Doppler.
During the assessment, you’ll observe the fetal heart rate, rhythm, and intensity.
What to look for when you are monitoring FHR intermittently:
- Increase in fetal heart rate to over 160 bpm
- Decrease in fetal heart rate to less than 110 bpm
- Fetal heart rate takes a long time to come back to its normal rate after the contraction passes off
- Irregular rhythm
The Benefits of intermittent fetal heart rate monitoring include:
- can detect baseline fetal heart rate, rhythm, and changes from baseline
- mobility for the mother in the first stage of labor
- freedom of movement since she is not attached to a stationary electronic fetal monitoring device
The limitations of intermittent fetal heart rate monitoring include:
- Inability to detect variability and types of decelerations
- Any transient significant abnormality in between observations are likely to be overlooked
- Inherent human error
- Sometimes difficult to count the fetal heart rate during uterine contractions or in case of obesity or hydramnios
2. Continuous Electronic Fetal Monitoring
As the name states, it is continuously monitoring fetal behavior using an electronic device during labor. This Electronic Fetal Monitoring (EFM) is called Cardiotocography (CTG). It traces both the fetal heart rate, fetal movement, and uterine contractions on a graph paper.
This can be done either using invasive or non-invasive devices.
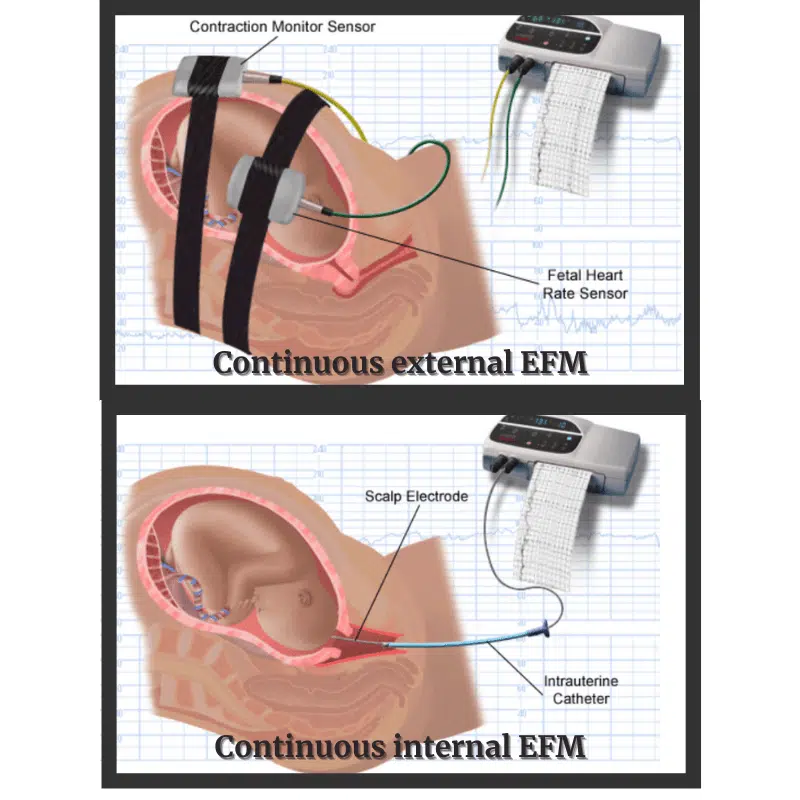
i. Non-invasive or external EMF
Non-invasive continuous motoring can be done externally by placing transducers on the mother’s tummy. A belt is used to secure these transducers.
The machine have two transducers. One is called toco-transducer. It records uterine contractions.
The other one is called an ultrasound transducer. And it records baseline FHR, long-term variability, accelerations, and decelerations.
Placement of non-invasive transducers
Toco-transducer – placed over the uterine fundus in the area of greatest contractility to monitor uterine contractions.
Ultrasound transducer – placed over mother’s abdomen in the midline between the umbilicus and the symphysis pubis.
The diaphragm of the ultrasound transducer is moved to either side of the abdomen to obtain a stronger sound.
ii. Invasive or internal EMF
Invasive EMF is done by applying a spiral pointed scalp electrode to the fetal scalp after rupturing the membranes. Intrauterine pressure could be simultaneously measured by passing a catheter inside the uterine cavity.
The fetal spiral electrode is the most accurate method of detecting fetal heart characteristics and patterns because it involves directly receiving a signal from the fetus.
Invasive EMF is used for high-risk mothers or fetuses.
Indication for Continuous Electronic Fetal Monitoring (EMF)
Continuous electronic fetal monitoring may be indicated due to maternal or fetal conditions. It is listed below.
Maternal conditions include:
- Hypertension
- Previous cesarean delivery
- Induced labor
- Antepartum haemorrhage (APH)
- Premature rupture of membrane (PROM)
Fetal conditions include:
- Small fetus (IUGR)
- oligohydramnios
- multiple pregnancies
- abnormal FHR on auscultation
Benefits of electronic fetal monitoring include:
- Accurate monitoring of uterine contractions
- Significant improvement of perinatal mortality
- Can detect hypoxia early
- Significant reduction in intrapartum fetal death rate
Disadvantages of this method include:
- Interpretation is affected by intra- and interobserver error
- Due to errors of interpretation, the cesarean section rate may be increased
- Instruments are expensive and trained personnel are required to interpret a trace
- Mother has to be confined in bed
CLICK HERE for a sample nursing care plan for Preeclampsia
How to locate the fetal heart sound during intrapartum?
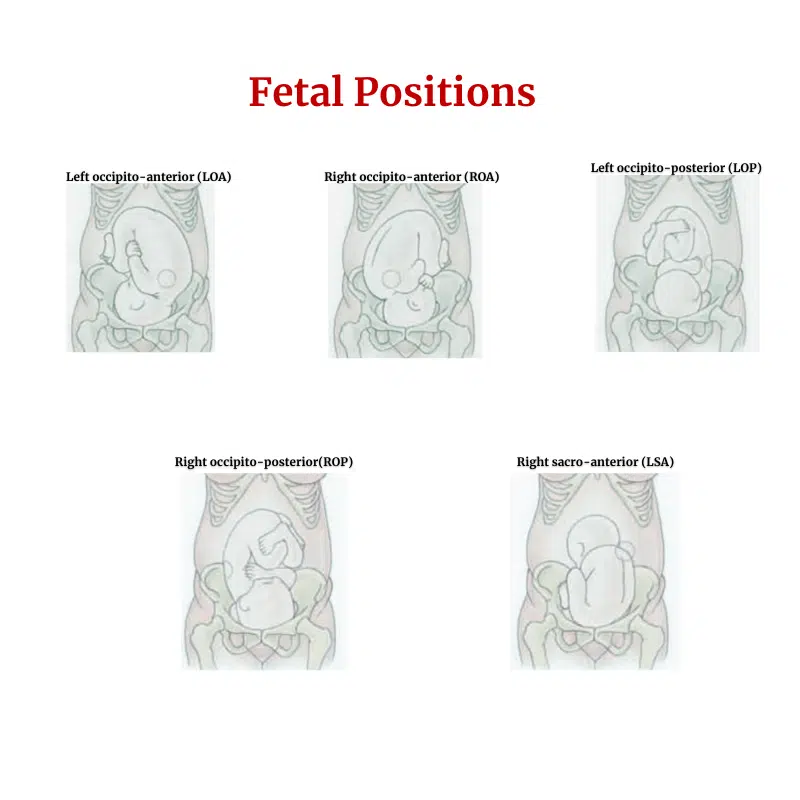
The back of the fetus is where you’ll hear FHR most clearly. Use Leopold’s maneuvers to locate the back of the fetus.
In a cephalic presentation, the FHR is best heard in the lower quadrant of the mother’s abdomen.
In a breech presentation, it is heard at or above the level of the mother’s umbilicus.
As labor progresses, the FHR location will change accordingly as the fetus descends lower into the mother’s pelvis for the birthing process.
What is “VEAL CHOP MINE” in Nursing?
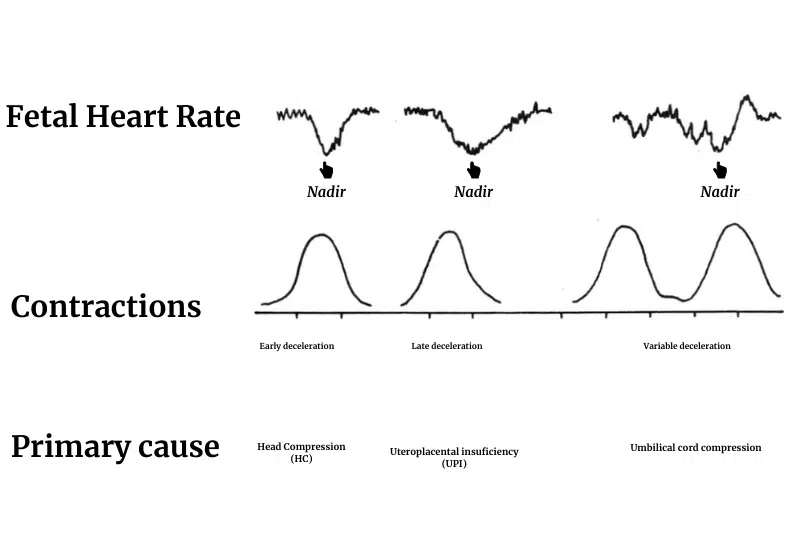
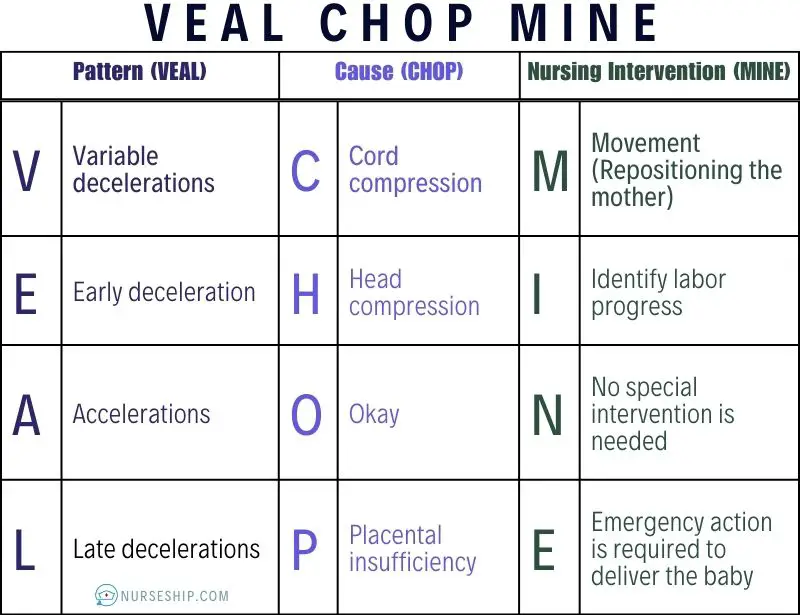
In nursing “VEAL CHOP MINE” is used as an acronym to remember fetal heart rate variability and patterns during intrapartum monitoring.
The first word “VEAL” denotes patterns of fetal heart rate. Secondly, the word “CHOP” represents the cause of these pattern variations.
Finally, “MINE” is for the nursing interventions required as per assessment findings.
VEAL CHOP MINE is further described in the table below.
| Pattern | Cause | Nursing Intervention |
|---|---|---|
| V = Variable decelerations | C = Cord compression | M = Movement (Repositioning the mother) |
| E = Early deceleration | H = Head compression | I = Identify labor progress |
| A = Accelerations | O = Okay | N = No special intervention is needed |
| L = Late decelerations | P = Placental insufficiency | E = Emergency action is required to deliver the baby |
Nursing Responsibilities:
- Observe for any change in maternal condition, such as ruptured membranes or the onset of bleeding.
- Assessing FHR at 30-minute intervals initially followed by 15-minute intervals in the first stage.
- Assessing FHR every 5 minutes in the second stage.
- Assess FHR for 60 seconds before and immediately following a uterine contraction. From then on, unless there is a problem, listening for 30 seconds and multiplying the value by two is sufficient.
Additional Sources
American College of Obstetricians and Gynecologists
National Institutes of Health (NIH)
Reference
Konar, H. (2015). DC Dutta’s textbook of obstetrics (8th ed). JP Brothers Medical.

Comments are closed.