In this article, you will review the types/classifications of fractures, 5 stages of bone healing process, and 5 P’s in nursing assessment of a patient with a fracture.
Quiz Your Nursing Fundamentals Knowledge Here
Also, you will learn about factors affecting bone healing, causes of fracture, signs, and symptoms, and complications.
What is a fracture in nursing?
A fracture is a traumatic break of the continuity of the bone. Fracture occurs when a bone is subjected to more stress than it can withstand.
Nursing care for fractures focuses on patient safety, preventing further injury, relieving pain, assisting with self-care, education, and promoting rehabilitative efforts to regain mobility and function.
Definition
Fracture is defined as a complete or incomplete disruption in the continuity of bone structure and is classified according to its type and extent.
What are the types/classification of fractures?
There are many types of fractures. And classification of fractures is also done in several ways.
A fracture can be classified based on the extent of the break. i.e.,
- Complete fracture (bone is completely separated at the point of fracture)
- Incomplete fracture (bone is partially separated at the point of fracture)
A fracture is also classified based on the degree of underlying soft tissue damage. i.e.,
- Closed fracture (or simple fracture): Fracture is enclosed inside skin tissue and has no visible wound.
- Open fracture (or compound fracture): Fracture penetrates the skin surface and the wound is visible at the site of injury.
Additionally, classification of fractures is done according to their cause. i.e.,
- Pathologic fracture (or spontaneous fracture): Occurs when bones become weak as a result of disease, such as metastatic cancer.
- Fatigue fracture (or stress fracture): Occurs due to repetitive stress. Commonly seen in athletes.
- Compression fracture: a fracture caused by pressing two bones together. They are extremely painful and commonly occur in the vertebrae of older patients with osteoporosis.
Following are the types of fractures based on their pattern of break.
- Spiral/ torsion fracture: Caused by twisting motion
- Greenstick fracture: Complete fracture on one side of the bone, and a bend on the other. Usually occur in children.
- Oblique fracture: Angular fracture (diagonal) line across a bone.
- Transverse fracture: Break across the bone, with the fracture at a right angle with the long axis of a bone.
- Linear fracture: Break along the vertical axis of the bone.
- Dislocation: Simultaneous occurrence of both fracture and dislocation.
- Comminuted/multi-fragmentary: Bone broken into more than three fragments, with no contact between distal and proximal fragments.
- Depressed fracture: Fragments are driven inwards; this happens mostly with fractures of the skull and facial bones.
- Avulsion fracture: A fragment of the bone is torn away, as seen with accidents that involve the tendon.
- Impacted fracture: occurs when bone fragments are wedged into other bone fragments.
In children, fracture is classified according to anatomical position. They include:
- Physis: the growth plate of a bone found in children, factures on this area are referred to as “physeal fractures”
- Epiphysis: Distal bone surface, that articulates with the joint, fractures occurring in the epiphysis are called “epiphyseal fractures”
- Metaphysis: Found between the epiphysis and shaft, and form a flare-like shape. Fractures in this area are referred to as “metaphyseal fractures”
- Diaphysis: The shaft of the long bone. Fractures in this area are referred to as “diaphyseal fractures”. They can either be proximal, middle, or distal.
Challenge Yourself With Our Quizzes
5 Stages of bone healing process
When a bone is fractured, the body immediately begins the healing process. The process of bone healing is described in several ways.
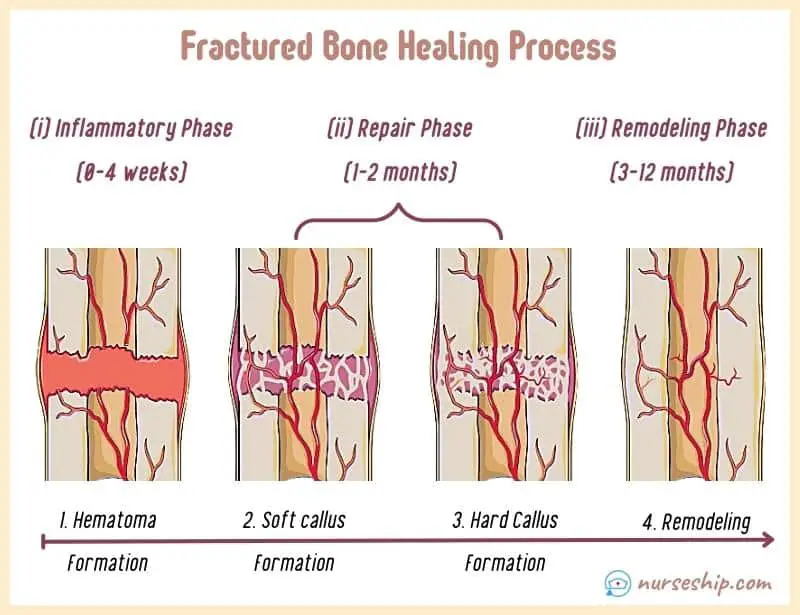
For example, the bone healing process is sometimes described in three phases as well. They are:
- Inflammatory phase [initial 4 weeks];
- Repair phase [1–2 months]; and
- Remodeling phase [up to 12 months].
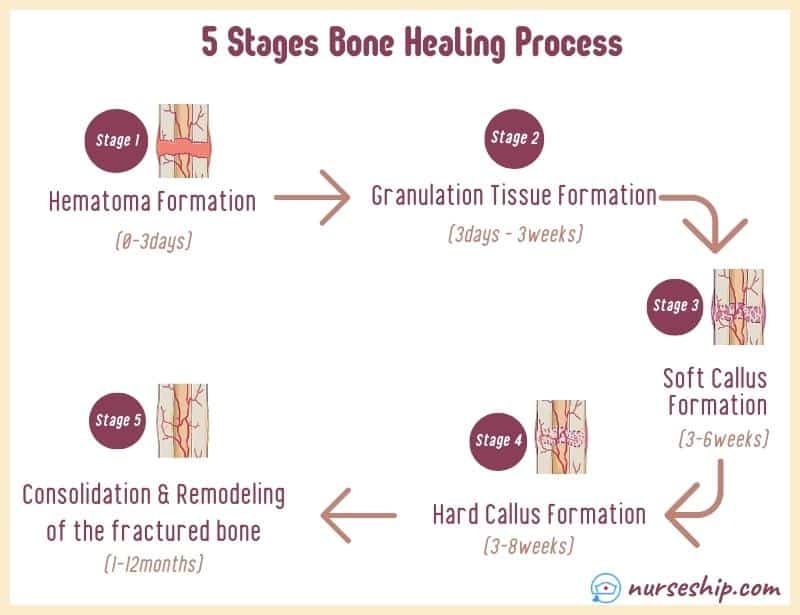
Following are the five stages of bone healing process in chronological order.
Bone healing process: Stage 1
Stage one is from 1-3 days after the injury. During this stage a hematoma forms at the site of the fracture.
Bone healing process: Stage 2
Stage two of bone healing occurs within 3 days to 3 weeks. During this stage granulation tissue begins to invade the hematoma.
This causes the formation of fibrocartilage, which serves as the foundation for bone healing.
Bone healing process: Stage 3
Stage three of bone healing occurs within 3 to 6 weeks after the injury. During this stage, vascular and cellular proliferation takes place, causing the formation of fibrocartilaginous callus.
The formation of new vascular tissue at the site of the fracture is called Callus. A nonbony union starts with soft callus formation.
Bone healing process: Stage 4
The fourth stage of the bone healing process lasts anywhere between 3 to 8 weeks.
At this stage, endochondral ossification (callus calcification process) takes place.
In which, the fibrocartilaginous callus is gradually replaced by mature bone, and the extra callus is gradually reabsorbed by osteoclasts.
Bone healing process: Stage 5
Stage five completes the bone healing process by remodeling and consolidating the fractured bone.
The final stage may start as early as 4 to 6 weeks after the fracture and can last up to a year.
The duration will depend on the severity of the injury, age, and general health of the patient.
What are the factors affecting bone healing?
Some of the factors affecting bone healing include:
- Age (bone heals faster in children while it is delayed in adults over 45 years)
- Presence of chronic diseases (such as HIV, diabetes, and cancer)
- Alcohol use
- Postmenopausal women
- Low body mass index (BMI)
- Malnutrition
- Smoking
- Use for certain medications (such as glucocorticoids)
- Infection
- Malignancy
- Misalignment
- Inadequate or improper immolation
- Avascular necrosis
- Bone loss
What are the five P’s in nursing assessment of a patient with a fracture?
Five P’s are acronyms used in the neurovascular assessment. The 5 P’s stands for Pain, Pulse, Pallor, Paresthesia, and Paralysis.
Nurses use the 5 P’s to assess fracture patients’ peripheral tissue perfusion and early detection of compartment syndrome.
Compartment syndrome is a complication of fracture which requires immediate medical attention. Because it can result in permanent muscle and nerve damage, as well as death.
paresthesia (nerve damage) and paralysis (disruption of nerves)

1. Pain
Assess pain using a pain assessment tool such as OLD CARTS. Also, use a standardized tool to determine the severity of the pain perceived by the patient.
2. Pulse
Assess the characteristics of the pulse distal to the fracture for quality, rate, and rhythm. Grade the pulse using a scale from 0 to 4+ (0 indicates no pulse and 4+ indicates bounding pulse).
3. Pallor
Pallor or paleness distal to the fracture indicates reduced blood flow. When the blood flow is interrupted, skin discoloration (bluish or purplish) and increased capillary refill can be observed.
4. Paresthesia
Paresthesia indicates damage to the nerves. The patient may complain of numbness, tingling, or pin or needles pricking sensation injured limb.
5. Paralysis
Paralysis is defined as the inability to move a fractured limb.
What are the causes of fractures?
Some of the causes of fracture include:
- Trauma (such as road traffic accidents, blunt/penetrating injuries, falls, sports-related injuries, and natural disasters).
- Osteoporosis (Which affects bone density. Spine, hip, and wrist fractures are common with osteoporosis).
- Repetitive stress, associated with occupational and sports/athletics.
- Malignant or benign bone tumors
- Osteomyelitis
Signs and symptoms
Following are the signs and symptoms of fracture.
- Pain
- Loss of function
- Deformity
- Swelling
- Bleeding
- Ecchymosis
- Crepitus
- Shortening of the affected limb
Take Our FREE NCLEX-Style Musculoskeletal System Quiz Here – Assess Your Knowledge
Complications of fracture
Complications can either be early or delayed.
Early complications include:
- Hypovolemic shock
- Rhabdomyolysis (breakdown of muscle tissue and subsequent release of myoglobin into circulation)
- Fat embolism
- Deep vein thrombosis (DVT)
- Disseminated intravascular coagulation (DIC)
- Bacterial infections
- Compartment syndrome (a medical emergency)
Delayed complications include:
- Complex regional pain syndrome (abnormally severe pain and reduced function that develops following injury)
- Delayed union (healing taking longer than expected)
- Malunion (bone healing but not in the right position)
- Nonunion (ends of the fractured bone failing to unite)
- Avascular necrosis
- Osteomyelitis
- Heterotrophic ossification
Conclusion
To sum up, 5 stages of bone healing process include (1) hematoma formation, (2) granulation tissue, (3) callus formation, (4) ossification, and (5) remodeling and consolidation of the bone.
The 5 P’s in nursing assessment of a patient with a fracture are (1) pain, (2) pulse, (3) pallor, (4) paresthesia, and (5) paralysis.
Reference
Hinkle, J., & Cheever, K. (2018). BRUNNER & SUDDARTH’S TEXTBOOK OF Medical-Surgical Nursing (14th ed.). Wolters Kluwer.
Hickman, R., Alfes, C. M., & Fitzpatrick, J. J. (2018). Handbook of clinical nursing. Medical surgical nursing. Springer.
Ignatavicius, D., Workman, M., Blair, M., Rebar, C., & Winkleman, C. (2016). Medical-Surgical Nursing Patient-Centered Collaborative Care (8th ed.). Elsevier.