Last updated on December 28th, 2023
In nursing, the term chronic kidney disease (CKD) refers to progressive, irreversible kidney damage or a decrease in the glomerular filtration rate (GFR) that lasts for three months or longer.
CKD is linked to lower quality of life, higher healthcare costs, and premature death. Untreated CKD can progress to end-stage kidney disease (ESKD) (aka, end-stage renal disease [ESRD]) the terminal stage of the disease.
ESRD causes uremic waste product retention and necessitates renal replacement therapy, dialysis, or kidney transplantation.
In this post, you will find 20 NANDA-I nursing diagnosis for chronic kidney disease (CKD). These include actual and risk nursing diagnoses.
CKD nursing assessment, interventions, priorities, and patient teaching are all included.
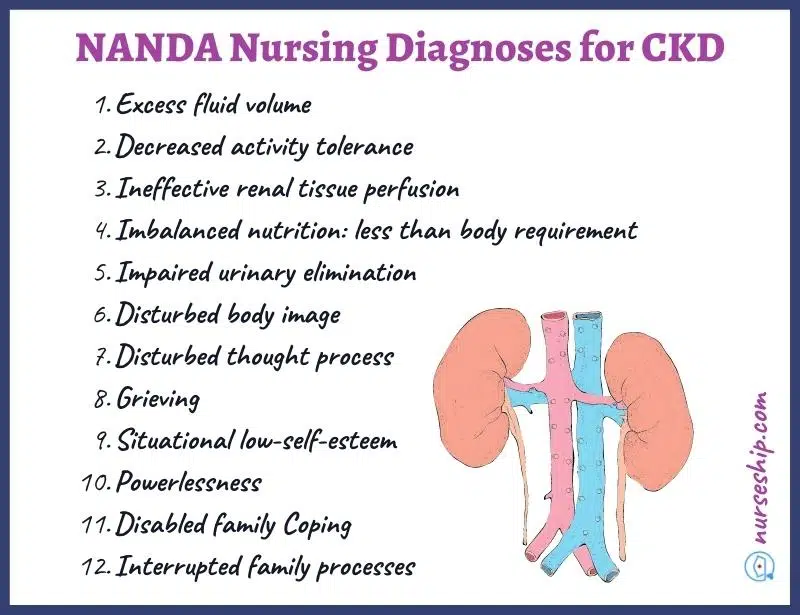
20 NANDA nursing diagnosis for chronic kidney disease (CKD)
- Excess fluid volume
- Decreased activity tolerance
- Ineffective renal tissue perfusion
- Imbalanced nutrition: less than body requirement
- Impaired urinary elimination
- Disturbed body image
- Disturbed thought process
- Grieving
- Situational low-self-esteem
- Powerlessness
- Disabled family Coping
- Interrupted family processes
- Risk for decreased Cardiac Output
- Risk for bleeding
- Risk for impaired oral mucous membrane integrity
- Risk for impaired skin integrity
- Risk for injury
- Risk for infection
- Risk for electrolyte imbalance
- Risk for acute confusion
Sample nursing care plan for acute renal failure
NANDA nursing diagnosis for Chronic Kidney Disease
#1 Excess fluid volume
| May be related to | As evidenced by |
| increased sodium retention, kidney dysfunction, compromised regulatory mechanism | Pulmonary congestion, jugular vein distension, oliguria <30ml/hr, edema, altered urine specific gravity, imbalanced intake, and output |
#2 Decreased activity tolerance
| May be related to | As evidenced by |
| Generalized weakness, imbalance between oxygen supply and demand | Fatigue on exertion, breathlessness, reluctance to perform activities of daily living (ADL), lack of energy, loss of vigor, lack of endurance |
#3 Ineffective renal tissue perfusion
| May be related to | As evidenced by |
| Impaired renal function | Elevated BUN, creatinine, uric acid and eGFR levels, anuria, oliguria, hypertension, muscle twitching and cramping, fatigue, weakness |
#4 Imbalanced nutrition: less than body requirement
| May be related to | As evidenced by |
| Inability to ingest, digest, or absorb food and nutrients | Fatigue, pallor, loss of muscle mass |
#5 Impaired urinary elimination
| May be related to | As evidenced by |
| Glomerular malfunction secondary to renal failure | Urinary retention, oliguria, anuria, dysuria, elevated BUN, and creatinine |
#6 Disturbed body image
| May be related to | As evidenced by |
| Presence of fistula, loss of weight, dry skin, facial puffiness | Hiding affected body parts, verbal detachment, self-isolation, refusal to talk about physical changes |
#7 Disturbed thought process
| May be related to | As evidenced by |
| Metabolic acidosis, hypoxia, electrolyte imbalances | Disorientation to place., person and time, irritability, altered attention span, impaired ability to make decisions, somnolence, inability to grasp ideas, withdrawal, depression |
#8 Grieving
| May be related to | As evidenced by |
| Chronic debilitating illness, loss of control | Expressions of anger, crying, sadness, alterations in sleep patterns, activity, eating or libido |
#9 Situational low-self-esteem
| May be related to | As evidenced by |
| Threat of death, loss of control, changes in family role and function | Expressions of helplessness or uselessness, self-negating behavior, indecisiveness |
#10 Powerlessness
| May be related to | As evidenced by |
| Chronic debilitating condition, threat of death, loss of control | Expressions of helplessness or uselessness, self-negating behavior, indecisiveness |
#11 Disabled family Coping
| May be related to | As evidenced by |
| Chronic debilitating condition, changes in family roles, changes in economic status | Expression of sadness over the way the family is acting and lack of their support, feeling of rejection, abandonment, and desertion, agitation, hostility, depression |
#12 Interrupted family processes
| May be related to | As evidenced by |
| Changes in health status, changes in family roles, modification in family finances | Reports of conflict within family, changes in communication and decision-making process, somatic complaints |
#13 Fatigue
| May be related to | As evidenced by |
| Anemia, reduced energy production | Shortness of breath, dyspnea, decreased oxygen saturation levels with movement or activity, increased heart rate and blood pressure with movement or activity, feelings of tiredness and weakness |
#14 Anxiety
| May be related to | As evidenced by |
| Change in health status, economic status, relationships, and role function; threat of death, lack of knowledge about diagnostic tests, disease process, treatment | Agitation, irritability, muscle tension, apprehension, communication of uncertainty, worry, sense of impending doomy |
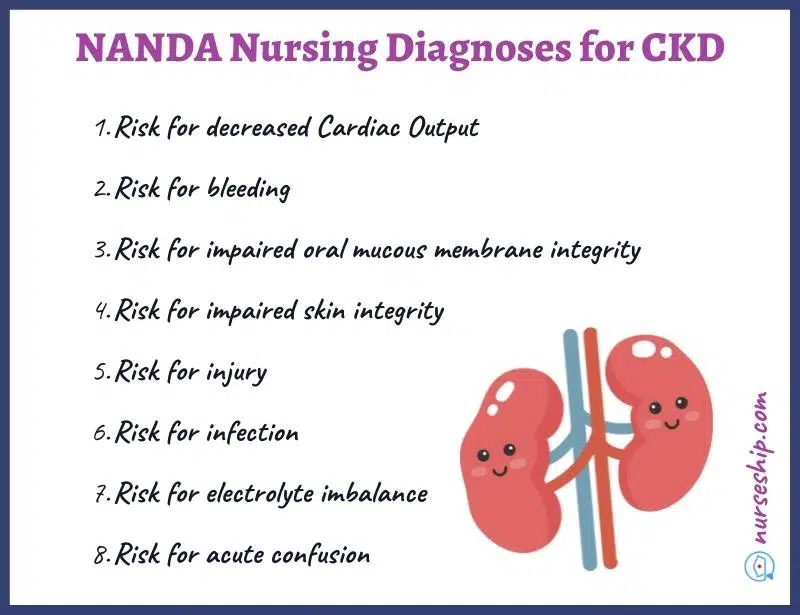
Risk nursing diagnosis for chronic kidney disease (CKD)
#1 Risk for decreased Cardiac Output
Associated risk factors
- Reduced stroke volume.
- Dysrhythmias
- Fluid overload
- Systemic vascular resistance (SVR)
- Electrolyte imbalances
#2 Risk for bleeding
Associated risk factors
- Altered erythropoietin production or secretion
- Reduced RBC production and their lifespan
- Altered blood clotting factors
#3 Risk for impaired oral mucous membrane integrity
Associated risk factors
- Decreased salivation
- Poor oral hygiene
- Dehydration
- Accumulation of toxins
#4 Risk for impaired skin integrity
Associated risk factors
- Skin breakdown
- Immune-related kidney dysfunction
- Malnutrition
- Altered peripheral sensation
- Accumulation of toxin in the skin
#5 Risk for injury
Associated risk factors
- Altered immune function
- Invasive procedures
- Kidney disease’s effects on bone density
- Altered blood clotting
- Altered drug elimination
#6 Risk for infection
Associated risk factors
- Altered functioning of the immune system
- Presence of comorbidities
- Uremia
- Dialysis access
#7 Risk for electrolyte imbalance
Associated risk factors
- Renal dysfunction
- Compromised regulatory mechanism
#8 Risk for acute confusion
Associated risk factors
- electrolyte imbalance
- Increased levels of BUN and/or creatinine
- Azotemia
Nursing priorities chronic kidney disease
- Prevent or delay the progression of the disease
- Prevent or minimize disease and treatment complications
- Patient education to promote physical and psychosocial well-being
Nursing management for chronic kidney disease (CKD)
CKD nursing assessment
- Obtain a complete patient history (such as medical, surgical, and psychosocial)
- Assess vital signs including body weight
- Assess kidney function (such as BUN, Creatinine, GFR) and need for dialysis
- Assess the effects of chronic renal failure (CRF) on other organs
- Assess the patient’s urinary output and the characteristics of the urine
- Assess for peripheral edema
- Assess nutritional status and dietary habits
- Assess the patient and family’s understating of CRF and treatment regimen
CKD nursing interventions
- Maintain intake and output chart
- Monitor daily body weight
- Monitor patient’s mental status
- Observe signs of fluid overload (such as lung crackles, pitting edema, distended neck veins, rapid bounding pulse, decreased O2 saturation).
- Monitor levels of BUN, Creatinine, GFR, serum osmolality, electrolytes, bicarbonate, pH, serum calcium, CBC, urinalysis.
- Monitor adherence to drug therapy, nutritional therapy, and fluid restriction.
- Prepare the patient for dialysis as needed
- Provide psychosocial support
Patient teaching for Chronic Kidney Disease
- Educate the patient regarding the disease process and treatment plan
- Inform the patient about the complications of CRF and treatment
- Teach the patient how to measure blood pressure and the importance of maintaining blood pressure and daily weight chart.
- Emphasize on the importance of controlling blood pressure and blood sugar levels to delay the progression of CKD.
- Explain the importance of adhering to the treatment regimen.
- Teach the patient about nutritional needs and essential dietary changes (such as low sodium, low potassium, limited fluid intake).
- Explain methods of psychological coping and how to get help.
- Explain the procedures for getting social and financial support.
Sample nursing care plan for acute renal failure
Chronic Kidney Disease (CKD) Review
CKD Definition
Chronic kidney disease (CKD) can be defined as progressive, irreversible kidney damage or decreased glomerular filtration rate (GFR) that lasts for three months or longer.
Stages of chronic kidney disease
The stages of CKD are determined according to estimated glomerular filtration rate (eGFR) levels.
The normal eGFR is 125 mL/min/1.73 m2.
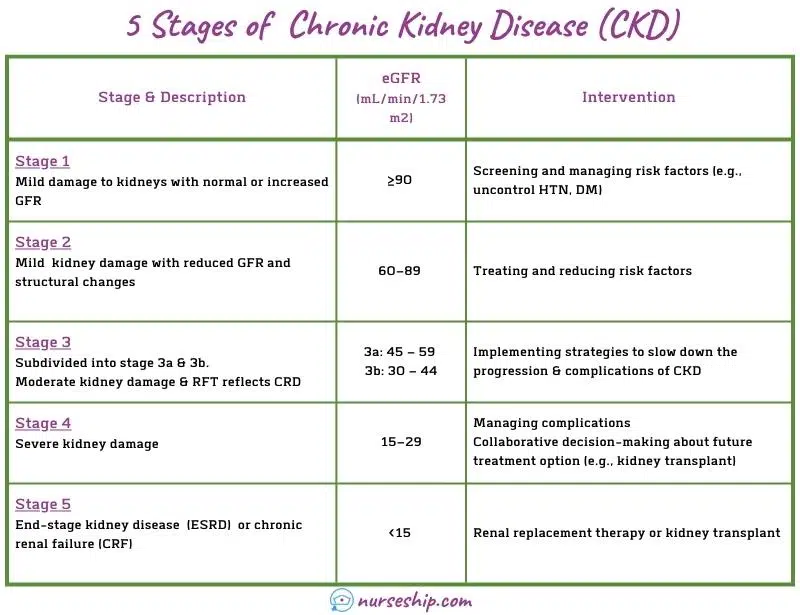
Stage 1 of CKD
The stage one of kidney disease, an individual may have a normal GFR (more than 90 mL/min/1.73 m2). But urine results, structural abnormalities, or genetic characteristics indicate kidney disease.
Stage 2 of CKD
GFR is decreased to 60–89 mL/min/1.73 m2 and mild kidney damage has occurred in the second stage of CKD.
Nephron loss may have resulted in small increases in metabolic waste levels in the blood. However, BUN, serum creatinine, uric acid, and phosphorus concentrations are not sensitive enough to identify this stage.
At this stage of CKD, there may be an increase in the flow of diluted urine, which can lead to severe dehydration.
Stage 3 of CKD
Stage 3 of CKD is further subdivided based on GFR levels. They are:
- Stage 3a: GFR 45 – 59 mL/min/1.73 m2.
- Stage 3b: GFR 30 – 44 mL/min/1.73 m2.
Kidney damage has progressed to a moderate level and symptoms may start manifesting at this stage. Other organs are also affected due to increased metabolic waste buildup in the blood.
Stage 4 of CKD
In stage 4 of CKD, GFR is decreased to 15–29 mL/min/1.73 m2 indicating severe kidney damage.
Renal function is severely impaired at this stage. The signs of other organ damage due to increased metabolic waste buildup in the blood are apparent.
Stage 5 of CKD
Stage five of chronic kidney disease refers to the end-stage of renal disease (ESRD) also known as “chronic renal failure.”
ESRD or stage 5 indicates that the renal failure has progressed to the point that it requires dialysis or a renal transplant to maintain life.
Prevalence and incidences
Kidney diseases are the leading cause of death in the United States. The CDC estimates that 15% of adults in the US (about 37 million people) have chronic kidney disease.
- The prevalence of CKD is higher in those 65 years and older (38%) compared to those 45 to 64 years (12%) and 18 to 44 years (6%).
- Women have a slightly higher prevalence of CKD than men, 14% and 12% respectively.
- Up to 90% of adults with CKD are unaware of their condition.
- Nearly 25% of persons with severe CKD are unaware of their condition.
CKD risk factors
- Uncontrolled hypertension
- Diabetes mellitus
- Chronic renal or urinary tract infection
- Family history of genetic renal disease
- Exposure to nephrotoxic substances
- Age over 65 years
Causes of CKD
There are more than 100 disease processes that cause progressive kidney disease. The main causes of CKD leading to dialysis are uncontrolled hypertension and diabetes.
Following are some of the causes of chronic kidney disease.
- Urinary tract diseases (such as obstructive uropathy)
- Glomerular diseases (such as glomerulonephritis)
- Tubular diseases (such as hypercalcemia)
- Vascular diseases of the kidney (such as bilateral renal artery stenosis)
- Genetic or inherited conditions (such as hypoplastic kidneys)
- Infections (such as pyelonephritis)
- Systemic vascular diseases (such as internal renovascular hypertension)
- Metabolic kidney diseases (such as amyloidosis, diabetes)
- Connective tissue diseases (progressive systemic sclerosis)
Signs and symptoms of CKD
Early CKD has no signs or symptoms. However, certain blood and urine markers (such as serum creatinine, BUN, proteinuria) are elevated.
As the kidney disease progresses, symptoms appear as a consequence of renal function impairment.
Signs and symptoms of stage 3
Some of the signs and symptoms of stage 3 of CKD include:
- Fatigue
- Peripheral pitting edema
- Shortness of breath
- Pruritus
- Insomnia
- Increased urine output and urine may appear cloudy or darker in color.
- Cramps
Signs and symptoms of stage 4
Some of the signs and symptoms of stage 4 of CKD include:
- High blood pressure
- High blood glucose levels
- Low hemoglobin levels
- Hyperkalemia
- Hyperphosphatemia
- Metabolic acidosis
- Uremia
- Fatigue
- Lethargy
- Peripheral pitting edema
- Increased urine output (early stages)
- Decreased urine output (later stages)
- Muscle cramps
- Nausea vomiting
- Dry and itchy skin
Signs and symptoms of stage 5
Some of the signs and symptoms of stage 5 of CKD include:
- Paresthesia
- Changes in vision
- Peripheral pitting edema
- Oliguria
- Anuria
- Proteinuria
- Decreased skin turgor
- Yellow-gray pallor
- Dry skin
- Pruritus
- Ecchymosis
- Shortness of breath
Complications of CKD
- Some of the complications of chronic kidney disease are listed below.
- Anemia
- Pulmonary edema
- Peripheral edema
- Cardiomyopathy
- Hypertension
- Heart failure
- Uremic pericarditis
- Pericardial effusion
- Cardiac tamponade
- Cardiorenal syndrome
- Ataxia
- Uremic colitis
- Soft-tissue calcifications
Sample nursing care plan for acute renal failure
Conclusion
To sum up, you now know 20 NANDA-I nursing diagnosis for chronic kidney disease that you can use in your nursing care plans.
Additionally, you have also learned about nursing assessment, nursing interventions, nursing priorities, and patient teaching for CKD.
Reference
Ackley, B., Ladwig, G., Makic, M., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing Diagnoses Handbook: An Evidence-based Guide to Planning Care (12th ed.). Elsevier.
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, and outcomes. Elsevier Health Sciences.
Herdman, T., Kamitsuru, S. & Lopes, C. (2021). NURSING DIAGNOSES: Definitions and Classifications 2021-2023 (12th ed.). Thieme.
Hinkle, J., & Cheever, K. (2018). BRUNNER & SUDDARTH’S TEXTBOOK OF Medical-Surgical Nursing (14th ed.). Wolters Kluwer.
Ignatavicius, D., Workman, M., Blair, M., Rebar, C., & Winkleman, C. (2016). Medical-Surgical Nursing Patient-Centered Collaborative Care (8th ed.). Elsevier.
Swearingen, P. (2016). ALL-IN-ONE Nursing Care Planning Resource (4th ed.). Elsevier/Mosby.