Cellulitis is a bacterial infection that causes inflammation of the dermal and subcutaneous layers of the skin.
Cellulitis most frequently affects the periorbital area and limbs where the skin is damaged by blisters, surgical incisions, cuts, insect bites, or burns.
In this post, you will find 9 NANDA-I nursing diagnosis for Cellulitis. These include actual and risk nursing diagnoses.
Cellulitis nursing management and patient teaching are all included.
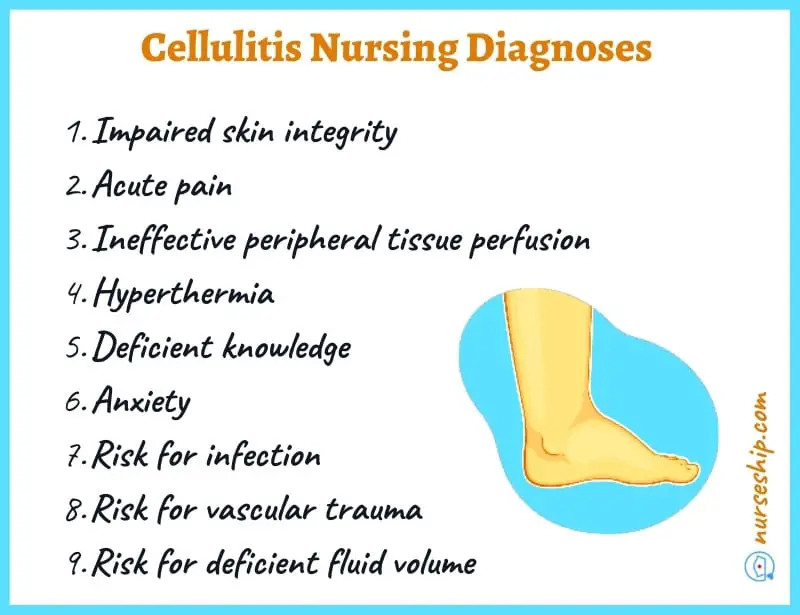
9 NANDA nursing diagnosis for Cellulitis
- Impaired skin integrity
- Acute pain
- Ineffective peripheral tissue perfusion
- Hyperthermia
- Deficient knowledge
- Anxiety
- Risk for infection
- Risk for vascular trauma
- Risk for deficient fluid volume
7 Actual Cellulitis nursing diagnoses
#1 Impaired skin integrity
| May be related to | As evidenced by |
| Trauma, surgical incision, thermal injury, insect bites | Open wound site, drainage of pus and lesions. |
#2 Acute pain
| May be related to | As evidenced by |
| Inflammatory process, circulating toxins, secondary to exogenous bacteria infiltration | Verbal reports of pain, facial grimace, guarding behavior, changes in vital signs, restlessness |
#3 Ineffective peripheral tissue perfusion
| May be related to | As evidenced by |
| Compromised blood flow to tissues secondary to cellulitis | Reduced sensation in extremities, acute pain, prolonged wound healing, swelling, redness |
#4 Hyperthermia
| May be related to | As evidenced by |
| Inflammatory process, response to circulatory toxins secondary to cellulitis | Increased body temperature above normal range, tachycardia, tachypnea, warm skin, flushed |
#5 Deficient knowledge
| May be related to | As evidenced by |
| New disease process, lack of understanding of the condition/treatment | Lack of adherence with treatment regimen and follow up, worsening of the condition, poor management of other risk factors |
#6 Anxiety
| May be related to | As evidenced by |
| Changes in health status, prolonged wound healing | Expression of worry and concerns, irritability, apprehension, muscle tension |
4 Risk nursing diagnosis for cellulitis
#1 Risk for infection
Associated risk factors
- Immunocompromised status
- Broken skin
- Chronic disease
- Presence of pathogens
- inadequate knowledge to avoid exposure to pathogens
#2 Risk for vascular trauma
Associated risk factors
- Prolong IV antibiotic therapy
#3 Risk for deficient fluid volume
Associated risk factors
- Increased body temperature
- Diaphoresis
- Insensible losses
- Inadequate fluid intake
Nursing management for Cellulitis
- Assess for pain, noting quality, characteristics, location, swelling, redness, increased body temperature.
- Assess the patient’s awareness of infection treatment, potential complications, the extent of cellulitis, and tissue perfusion.
- Obtain specimens for culture and sensitivity testing
- Monitor vital signs.
- Aseptic wound care
- Application of warm compression
- Administration of prescribed antibiotics and pain medications
- Monitoring for complications
- Screening the patient for risk factors
- Patient education on hand hygiene
- Patient family education on condition and management at home
- Documentation of interventions
Patient teaching for Cellulitis
- Hygiene practices
- Wound care
- Adherence to discharge medications
- Monitoring of temperature
- Elevation of affected limb
- Danger signs and symptoms of infection (such as, very high grade fever, confusion or disorientation, severe pain, dyspnea)
Cellulitis Review
What is Cellulitis?
Cellulitis is a condition affecting skin caused by exogenous bacteria whereby localized inflammation of the connective tissue occurs causing subsequent inflammation of the skin above (dermal and subcutaneous layers).
Cellulitis is most common in places (limbs)where the skin was broken before by blisters, surgical wounds, cuts, insect bites or burns.
Definition of cellulitis
Cellulitis is defined as a localized, bacterial-inflicted inflammation of the skin and subcutaneous tissue that spreads past the site of injury.
Pathophysiology of cellulitis
Initially, the causative organism enters the body through breaks of skin (such as cuts, insect bites, incisions, etc).
The inflammatory response then occurs, exhibiting the hallmark characteristics of cellulitis (i.e., redness, pain, hot skin, and swelling).
Cellulitis spreads beyond the invasion site, affecting dermal and subcutaneous tissues.
Cellulitis is most commonly caused by group A streptococci (Streptococcus pyogenes).
Risk factors
Cellulitis risk factors include:
- Immunocompromised health status due to comorbidities such as HIV/AIDS, diabetes, and cancer
- Chickenpox
- Shingles
- Injection drug use
- Skin conditions such as eczema
- Lymphedema
- Obesity
- Elderly
- Coronary artery bypass grafting
Signs and symptoms of cellulitis
- Redness
- Pain
- Hot skin
- Swelling
- Malaise
- Fever
- Purulent discharge
Complications
- Sepsis
- Bacteremia
- Osteomyelitis
- Infective endocarditis
- Suppurative arthritis
- Gangrene
Prognosis
Usually, the prognosis of cellulitis is good when treated early stages. However, if cellulitis is left untreated it can cause life-threatening complications such as sepsis.
See also:
Sample nursing care plan for hyperthermia
Risk for infection nursing care plans
Conclusion
To sum up, you now know 9 NANDA-I nursing diagnosis for Cellulitis that you can use in your nursing care plans.
Additionally, you have also learned about nursing management and patient teaching for cellulitis.
Reference
Ackley, B., Ladwig, G., Makic, M., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing Diagnoses Handbook: An Evidence-based Guide to Planning Care (12th ed.). Elsevier.
Carpenito, L. J. (2021). Handbook of nursing diagnosis. Jones & Bartlett Learning.
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, and outcomes. Elsevier Health Sciences.
Herdman, T., Kamitsuru, S. & Lopes, C. (2021). NURSING DIAGNOSES: Definitions and Classifications 2021-2023 (12th ed.). Thieme.
Hinkle, J., & Cheever, K. (2018). BRUNNER & SUDDARTH’S TEXTBOOK OF Medical-Surgical Nursing (14th ed.). Wolters Kluwer.
Ignatavicius, D., Workman, M., Blair, M., Rebar, C., & Winkleman, C. (2016). Medical-Surgical Nursing Patient-Centered Collaborative Care (8th ed.). Elsevier.
Swearingen, P. (2016). ALL-IN-ONE Nursing Care Planning Resource (4th ed.). Elsevier/Mosby.