Last updated on December 28th, 2023
In this post, you will find 19 NANDA nursing diagnosis for fracture. These include actual and risk nursing diagnoses.
Fracture nursing assessment, interventions, priorities, and patient teaching are all included.
In nursing, a fracture can be defined as a break in a bone due to direct or indirect pressure that exceeds the bone’s normal elasticity.
Fracture causes damage to surrounding soft tissues, nerves, tendons, and vasculature and is associated with severe pain and as well.
Click Here to Review Fracture Notes.
19 Fracture Nursing Diagnosis
- Acute pain
- Impaired physical mobility
- Impaired skin integrity
- Self-care deficit
- Disturbed body image
- Fear
- Deficient knowledge
- Impaired comfort
- Anxiety
- Risk for peripheral neurovascular dysfunction
- Risk for infection
- Risk for thrombosis
- Risk for impaired gas exchange
- Risk for ineffective peripheral tissue perfusion
- Risk for decreased cardiac tissue perfusion
- Risk for decreased cardiac output
- Risk for unstable blood pressure
- Risk for ineffective cerebral tissue perfusion
- Risk for imbalanced fluid volume
NANDA nursing diagnoses for Fracture (Actual)

#1 Acute pain
| May be related to | As evidenced by |
| Fracture, movement of bone fragments, soft tissue injury, vascular trauma, nerve injury, traction device, muscle spasms, tendon injury | Report of pain as severe on a standardized pain scale, crying, facial grimace, guarding behavior, diaphoresis, tachycardia, tachypnea, increased blood pressure |
#2 Impaired physical mobility
| May be related to | As evidenced by |
| Altered bone integrity, immobilization, traction device, decrease in muscle strength and control, neuromuscular impairment | Decreased range of motion, poor muscle control, muscle pull/spasm, reduced muscle strength, need for restriction of movement, postural instability |
#3 Impaired skin integrity
| May be related to | As evidenced by |
| Open fractures, internal/external fixation devices, traumatic injury, surgical intervention, prolonged immobilization | Open wound, surgical incision site, paresthesia, presence of pressure ulcers on bony prominences |
#4 Self-care deficit (Dressing/Bathing/Toileting)
| May be related to | As evidenced by |
| Immobilization, pain, limited range of motion (ROM) | Inability to perform activities of daily living (ADLs) independently, difficulty in putting on and removing clothes, difficulty in using assistive device, difficulty in walking |
#5 Disturbed body image
| May be related to | As evidenced by |
| Fracture(s), presence of immobilizing devices, amputation, tubes and drains | Verbal expression of negative feelings about injury, unhappiness, fear of rejection, unwillingness to meet people |
#6 Fear
| May be related to | As evidenced by |
| Impending surgical intervention, hospital environment, hospital procedures, orthopedic equipment | Verbal expression of fear, tensing of muscles, tachypnea, tachycardia, crying, insomina |
#7 Deficient knowledge
| May be related to | As evidenced by |
| Lack of factual information, presence of learning disability | Non-compliance with treatment, statement of inaccurate statement, inquiry about the condition, requests for information, development of preventable complications |
#8 Impaired comfort
| May be related to | As evidenced by |
| Cast application, internal fixation devices, restricted movement, | Presence of casts, reports of discomfort and altered sleep-wake cycle, difficulty in relaxing, irritability |
#9 Anxiety
| May be related to | As evidenced by |
| Surgery, hospitalization, acute change in health status | Reports of psychological distress, irritability, apprehension, agitation, altered sleep-wake cycle |
Risk nursing diagnosis for Fracture
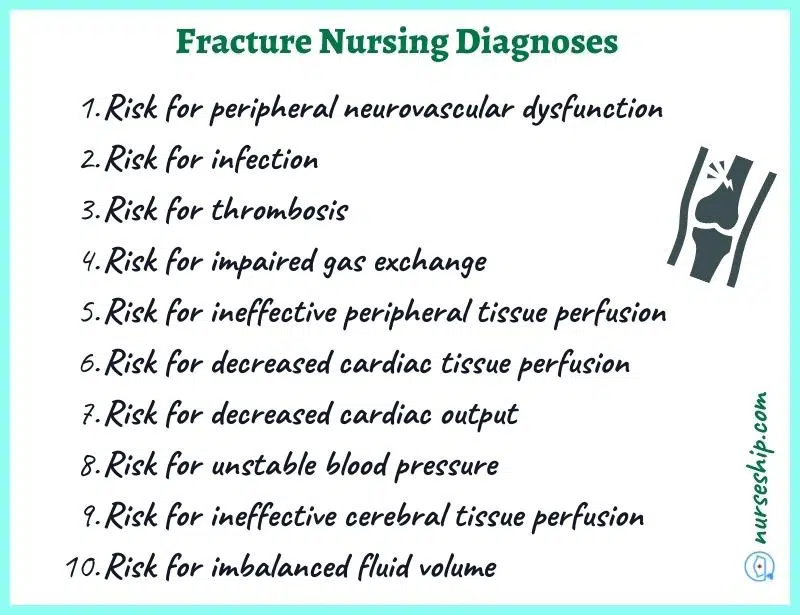
#1 Risk for peripheral neurovascular dysfunction
Associated risk factors
- Interrupted blood flow
- Thrombus formation
- Vascular and soft tissue injury
- Hypovolemia
#2 Risk for infection
Associated risk factors
- Impaired skin integrity
- Invasive procedures
- Prolonged hospital stay
- Traction devices
#3 Risk for thrombosis
Associated risk factors
- Presence of fracture
- Prolonged immobilization
- Surgical intervention
#4 Risk for impaired gas exchange
Associated risk factors
- Altered blood flow
- Presence of blood/fat emboli
- Pulmonary edema
- Pulmonary tissue trauma
#5 Risk for ineffective peripheral tissue perfusion
Associated risk factors
- Altered blood flow due to fracture
- Presence of casts
#6 Risk for decreased cardiac tissue perfusion
Associated risk factors
- Altered blood flow due to fracture
- Internal bleeding
#7 Risk for decreased cardiac output
Associated risk factors
- Decrease in circulatory blood volume due to hemorrhage
#8 Risk for unstable blood pressure
Associated risk factors
- Altered blood flow
- Internal bleeding
#9 Risk for ineffective cerebral tissue perfusion
Associated risk factors
- Altered blood flow
- Internal bleeding
#10 Risk for imbalanced fluid volume
Associated risk factors
- Internal bleeding
- Active bleeding
Nursing Priorities for Fractures
- Prevent further bone/tissue damage.
- Pain management
- Restoration of function
- Prevent infection and other complications
- Health education on fractures, pain management, immobilization, medical treatment, orthopedic device care, home care, and rehabilitation
Nursing Management for Facture
Nursing Assessment
- Asses pain: location, severity, duration, alleviating and aggravating factors
- Asses and monitor vital signs
- Asses muscle strength and ROM in unaffected joints
- Asses affected extremities regularly for signs of neurovascular compromise such as paresthesia, paralysis, weak and thread pulses and sluggish capillary refill.
- Obtain x-ray films to determine the extent of injury
5 P’s in Nursing Assessment of a Patient with a Fracture.
| Subjective data | Objective data |
| Localized pain (To fracture site) | Guarding behavior, restlessness, irritability, moaning and crying |
| Muscle spasms/ cramping on immobilization | Limited range-of-motion (ROM) |
| Gait and/or mobility problems | Discrepancy in limb length |
| Numbness or tingling (paresthesia) | Hypertension, tachycardia, diminished pulses, pallor |
| Fatigue and weakness | Loss of function of affected extremity |
Nursing Interventions
- Monitor circulation (check for changes in peripheral pulses, capillary refill, and skin temperature distal to the injury).
- Monitor vital signs (check for tachycardia, hypotension, tachypnea, and elevated body temperature)
- Administer analgesics, anticoagulants, and muscle relaxants as indicated
- Give/encourage analgesia 30-45 minutes before physiotherapy sessions
- Maintain immobilization while elevating affected extremity
- Apply non-pharmacological pain relief measures such as ice pack application, deep-breathing techniques
- Facilitate physiotherapy sessions as soon as possible (Early ambulation for better outcomes)
- Assist with range of motion (ROM) exercises as needed while encouraging independence.
- Monitor for signs of thromboembolisms
- Apply anti-embolic stockings or other compression devices as per institution’s protocol
Patient Teaching for Fracture
Patient teaching for fracture should include the following.
- Treatment regimen including medication doses, purpose, and possible side effects
- Non-pharmacologic methods to manage pain
- Limb elevation
- Proper use and care of orthopedic assistive devices, casts, etc.
- Self-initiated range of motion exercises
- Aseptic wound care
- Danger signs such as pus formation, severe pain, fever and chills, paresthesia and paralysis
- Importance of follow up, and provide a date and time for follow up.
Conclusion
To sum up, you now know 19 NANDA-I nursing diagnosis for fracture that you can use in your nursing care plans.
Additionally, you have also learned about nursing assessment, nursing interventions, nursing priorities, and patient teaching for bone fractures.
Reference
Ackley, B., Ladwig, G., Makic, M., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing Diagnoses Handbook: An Evidence-based Guide to Planning Care (12th ed.). Elsevier.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2013) Nurses pocket guide: Diagnoses, interventions, and rationales (13th ed.). F. A. Davis Company
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, and outcomes. Elsevier Health Sciences.
Herdman, T., Kamitsuru, S. & Lopes, C. (2021). NURSING DIAGNOSES: Definitions and Classifications 2021-2023 (12th ed.). Thieme.
Swearingen, P. (2016). ALL-IN-ONE Nursing Care Planning Resource (4th ed.). Elsevier/Mosby.


Comments are closed.