Last updated on December 28th, 2023
In this article, we will cover in-depth the Nursing Assessment, which is the very first step of the nursing process.
What is Nursing Assessment?
Nursing assessment involves a systematic and comprehensive approach in which nurses collect data on a patient’s physical, psychological, emotional, social, and environmental status.
Nursing assessment is essential for developing an accurate and holistic understanding of the patient’s health condition, needs, and potential risks.
Nursing assessment process serves as the foundation for creating a care plan and making informed clinical decisions.
Definition of Nursing Assessment
Nursing assessment can be defined as the collection of information from the patient and secondary sources (e.g., family members), as well as the interpretation and validation of that information, with the goal of establishing a complete database.
What is the Purpose of Nursing Assessment?
The primary purpose of nursing assessment is to establish a baseline database that reflects the patient’s perceived needs, health problems, and their corresponding responses.
This foundational knowledge serves as a baseline for developing individualized care plans, making well-informed clinical judgments, and facilitating effective communication among members of the healthcare team.
The initial nursing assessment also acts as a measure for assessing the effectiveness of the care being delivered.
Why is Nursing Assessment Important?
Nursing assessment is important because it establishes a baseline understanding of a patient’s condition, enabling accurate diagnosis, personalized care planning, and informed decision-making.
It helps detect issues early, supports effective communication among healthcare teams, and guides interventions.
Through assessment, nurses advocate for patients, ensure evidence-based care, and evaluate treatment outcomes.
In essence, nursing assessment is the foundation for delivering safe, effective, and patient-centered healthcare.
What are the 4 Types of Nursing Assessments?
The four types of nursing assessments can be classified based on the timing and purpose of the assessment. They are as follows:
1. Initial Assessment:
Initial Assessment is conducted shortly after a patient’s admission to a healthcare facility, the initial assessment aims to establish a comprehensive baseline of the patient’s health status, needs, and potential issues.
It provides a reference point for future comparisons and problem identification.
2. Problem-Focused Assessment:
Problem-Focused assessment is integrated into ongoing nursing care and is targeted at evaluating the status of a specific problem that was identified in a previous assessment.
It helps determine whether interventions are effectively addressing the identified issue.
3. Emergency Assessment:
Performed during physiological or psychological crises, emergency assessments aim to quickly identify any life-threatening problems or previously overlooked issues.
Emergency assessment is crucial for immediate decision-making and intervention.
4. Time-Lapsed Reassessment:
Conducted several months after the initial assessment, the time-lapsed reassessment involves comparing the patient’s current health status with the baseline data obtained earlier.
This helps track changes, improvements, or potential deterioration over time.
Examples of the 4 Types of Nursing Assessments
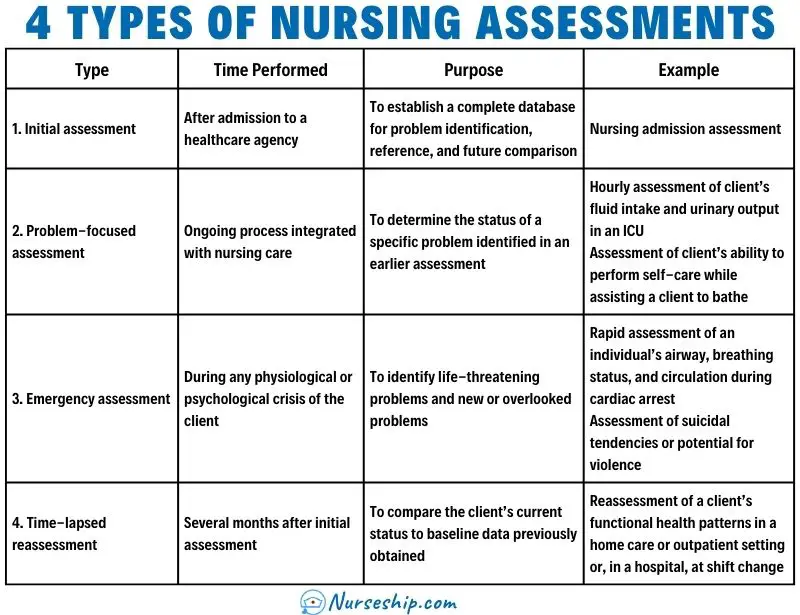
| Type | Time Performed | Purpose | Example |
| 1. Initial assessment | After admission to a healthcare agency | To establish a complete database for problem identification, reference, and future comparison | Nursing admission assessment |
| 2. Problem-focused assessment | Ongoing process integrated with nursing care | To determine the status of a specific problem identified in an earlier assessment | Hourly assessment of client’s fluid intake and urinary output in an ICU Assessment of client’s ability to perform self-care while assisting a client to bathe |
| 3. Emergency assessment | During any physiological or psychological crisis of the client | To identify life-threatening problems and new or overlooked problems | Rapid assessment of an individual’s airway, breathing status, and circulation during cardiac arrest Assessment of suicidal tendencies or potential for violence |
| 4. Time-lapsed reassessment | Several months after initial assessment | To compare the client’s current status to baseline data previously obtained | Reassessment of a client’s functional health patterns in a home care or outpatient setting or, in a hospital, at shift change |
What are the Steps in Nursing Assessment?
Nursing assessment involves a systematic approach to gathering information about a patient’s health status and needs. The steps in nursing assessment typically include:
- Data Collection
- Organizing Data
- Data Validation
- Documenting the Data
1. Data Collection
Data collection is a systematic continuous process of gathering information from various sources, including the patient, medical records, family members, and healthcare team.
What are the Types of Data
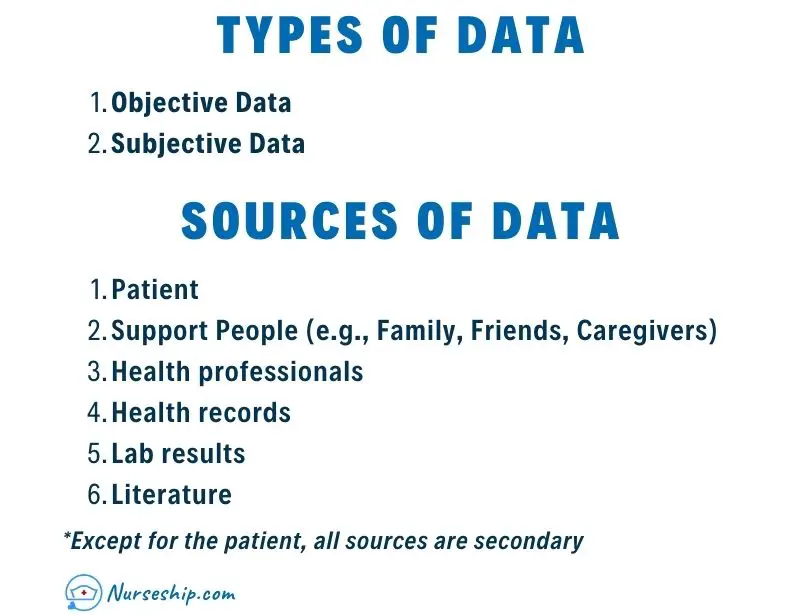
Subjective data, also known as covert or symptoms, are exclusive to the individual experiencing them and can only be described or confirmed by that person.
Examples of subjective data include itching, pain, and feelings of unease.
Objective data, also termed overt or signs, can be perceived by an observer, measured, or assessed against a recognized standard.
They are detectable through sight, sound, touch, or smell, and are collected through observation or physical examination.
Examples of objective data include skin discoloration, blood pressure, Pulse rate, etc.
Learn more about Subjective vs Objective Data
What are the Sources of Data?
Data sources are categorized into primary and secondary. The patient is the primary source, while family, health professionals, records, lab results, and literature are secondary.
Except for the patient, all sources are secondary. Validation is recommended for data from secondary sources.
What are the Methods of Data Collection?
- Observing,
- Interviewing, and
- Examining
The primary methods of data collection in nursing include observing, interviewing, and administering examinations.
The nurse uses these three methods simultaneously during the assessment process.
For example, during the interview to collect a patient’s health history, the nurse observes, listens, asks questions, and mentally retains information to be examined during the physical examination.
Learn More About Nursing Health History.
2. Organizing Data
Nurses organize assessment data in written or electronic formats known as nursing health histories, assessments, or database forms.
These formats can be adjusted based on the patient’s physical condition, like using a specific form for orthopedic patients focused on musculoskeletal data.
Many nursing schools and healthcare organizations have their own structured nursing assessment formats.
These are often influenced by specific nursing models such as Gordon’s functional health pattern framework, Orem’s self-care model, and Roy’s adaptation model.
3. Data Validation
During the assessment phase, gathered information must be complete, factual, and accurate as nursing diagnoses and interventions rely on it.
Validation, or double-checking data for accuracy, ensures completeness, agreement between objective and subjective data, and prevents oversight.
Validating data helps to:
- differentiate cues (observable data) from inferences (nurse’s interpretations),
- avoids mistaken conclusions, and
- focuses on the right problems.
Certain data, like measurable values, might not need validation, but discrepancies or varying client statements warrant validation.
Nurses need to be aware of biases, separate facts from assumptions and validate assumptions to build an accurate database, as failing to do so risks an incomplete and inaccurate nursing assessment that could compromise patient safety.
4. Documenting the Data
In the final step of the nursing assessment, the nurse meticulously records patient data, with accuracy and completeness being critical.
Objective, factual recording is emphasized, avoiding nurse interpretations. For example, breakfast intake is documented as specific items consumed, not subjective judgments like “appetite good.”
Subjective data are best captured using the client’s exact words in quotation marks, as paraphrasing risks altering their intended meaning.
See Also:
- What is Critical Thinking in Nursing? (Explained W/ Examples)
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
The Nursing Assessment FAQs
What is the Difference Between a Medical Assessment and a Nursing Assessment?
| Aspect | Medical Assessment | Nursing Assessment |
| Focus | Diagnosing and treating medical conditions. | Understanding holistic health status and needs. |
| Performed by | Medical doctors (physicians), advanced medical practitioners. | Nurses. |
| Emphasis | Medical conditions, diseases, physiological abnormalities. | Physical, psychological, emotional, social, and environmental aspects. |
| Scope | Primarily physical symptoms, diagnostic tests, medical interventions. | Broader: lifestyle, cultural beliefs, family dynamics, self-care ability. |
| Outcomes | Diagnosing and medically managing conditions. | Developing patient-centered care plans, comprehensive care. |
| Approach | Primarily physiological and disease-focused. | Holistic, considering patient’s overall well-being. |
| Intervention Focus | Medical treatments, medications, procedures. | Patient-centered care, comfort, well-being. |
| Goal | Restore patient’s health through medical interventions. | Provide comprehensive care, promote well-being. |
In summary, medical assessment primarily concentrates on diagnosing and treating medical conditions from a physiological perspective.
While nursing assessment focuses on understanding and addressing the patient’s holistic health needs to provide comprehensive care.
Both assessments contribute to a thorough understanding of the patient’s health and guide appropriate interventions from their respective perspectives.
What are the 4 Types of Physical Assessment?
The four main types of physical assessments are:
- Comprehensive Assessment: This is a detailed and thorough assessment of the patient’s overall health status. It involves a comprehensive examination of all body systems and is typically performed when a patient is admitted to a healthcare facility or during an annual check-up.
- Focused Assessment: A focused assessment is conducted to gather information about a specific problem or body system. It targets a particular area of concern, such as assessing the respiratory system in a patient with breathing difficulties.
- Ongoing or Routine Assessment: This type of assessment is performed regularly, often at specified intervals, to monitor a patient’s health status and track any changes. It is common in settings like hospitals or long-term care facilities to ensure that changes in the patient’s condition are detected early.
- Emergency Assessment: Emergency assessments are conducted during urgent situations when a patient is experiencing a medical crisis or emergency. The focus is on rapidly identifying life-threatening issues and stabilizing the patient’s condition.
What are the 5 Components of Nursing Assessment?
A nursing assessment typically includes the following five components:
- Biographical Data and Chief Complaint: Gathering basic information about the patient, such as age, gender, and reason for seeking healthcare, helps set the context for the assessment.
- Health History: This involves collecting detailed information about the patient’s medical history, past illnesses, surgeries, medications, allergies, family history, and lifestyle factors.
- Physical Examination: A thorough physical examination is conducted to assess the patient’s overall health, including vital signs, body systems, and any potential abnormalities or signs of illness.
- Review of Systems: This involves asking the patient about specific symptoms or experiences related to each body system, even if they are not directly related to the chief complaint, to identify any potential health issues.
- Psychosocial Assessment: Evaluating the patient’s psychological, emotional, and social well-being, including factors such as stressors, coping mechanisms, support systems, and cultural beliefs, helps provide holistic care.
These components collectively provide a comprehensive understanding of the patient’s health status and guide the development of an individualized care plan.
What is a Full Nursing Assessment?
A full nursing assessment can be described as a comprehensive process that involves gathering detailed biographical and health history information, conducting a thorough physical examination, reviewing the patient’s systems, and assessing their psychosocial well-being.
This holistic approach provides a comprehensive understanding of the patient’s health status, enabling the development of personalized care plans.
What is a Good Nursing Assessment?
A good nursing assessment is one that is thorough, accurate, holistic, and patient-centered. It involves systematically collecting comprehensive data about the patient’s physical, emotional, psychological, and social aspects.
A good nursing assessment considers the patient’s individual needs, preferences, and cultural background. It requires effective communication skills to build rapport and gather information, as well as critical thinking to analyze data and identify potential health issues.
A good nursing assessment serves as the foundation for informed clinical decisions, personalized care planning, and positive patient outcomes.
How Do You Assess a Patient?
Assessing a patient involves a systematic process that gathers information about the patient’s health status, needs, and preferences.
Here are the general steps to assess a patient:
- Preparation: Gather necessary tools (stethoscope, thermometer, etc.) and review the patient’s medical records and history.
- Introduction: Introduce yourself, establish rapport, and explain the purpose of the assessment.
- Obtain Biographical Data: Gather basic information like the patient’s name, age, gender, and reason for seeking healthcare.
- Chief Complaint: Ask the patient to describe their main reason for the visit or their primary health concern.
- Health History: Collect detailed information about the patient’s medical history, past illnesses, surgeries, medications, allergies, family history, and lifestyle factors.
- Physical Examination: Systematically examine the patient’s body systems, including vital signs (temperature, blood pressure, pulse, respiratory rate), using appropriate techniques and tools.
- Review of Systems: Ask the patient about symptoms or experiences related to each body system, even if they aren’t related to the chief complaint.
- Psychosocial Assessment: Assess the patient’s psychological, emotional, and social well-being, including stressors, coping mechanisms, support systems, and cultural beliefs.
- Validation: Compare data collected during the assessment for consistency and accuracy.
- Documentation: Accurately record assessment findings in the patient’s medical record, including both objective (observable) and subjective (patient-reported) data.
- Analysis and Interpretation: Analyze the collected data to identify potential health issues, formulate nursing diagnoses, and set priorities.
- Clinical Decision-Making: Based on the assessment data, make informed decisions about the patient’s care and determine the appropriate interventions.
- Communication: Share assessment findings with the healthcare team and collaborate on care planning.
- Patient Education: Communicate assessment results to the patient, explain findings, and educate them about their health status and care plan.
- Continuous Monitoring: Throughout the patient’s care journey, monitor their progress and reassess as needed.
What are Focused Assessment Nursing Examples?
A focused nursing assessment is tailored to address a specific issue, condition, or body system of concern for a patient.
Here are a few examples of focused assessments in nursing:
- Respiratory Assessment: Conducted on a patient with shortness of breath, the nurse assesses respiratory rate, lung sounds, oxygen saturation levels, and any signs of respiratory distress.
- Pain Assessment: For a patient experiencing abdominal pain, the nurse assesses the onset, location, intensity, quality, and factors that aggravate or alleviate the pain.
- Neurological Assessment: When a patient reports a sudden headache and confusion, the nurse assesses neurological function by evaluating the level of consciousness, motor function, sensory perception, and pupil reactions.
- Wound Assessment: For a patient with a surgical incision, the nurse assesses the wound site for signs of infection, redness, swelling, drainage, and overall healing progress.
- Cardiac Assessment: In response to a patient’s complaint of chest pain, the nurse assesses heart rate, blood pressure, electrocardiogram readings, and cardiac rhythm.
- Fluid Balance Assessment: For a patient with signs of dehydration, the nurse assesses intake and output, skin turgor, mucous membranes, and vital signs.
- Diabetic Assessment: When caring for a patient with diabetes, the nurse assesses blood glucose levels, signs of hyperglycemia or hypoglycemia, and any related complications.
- Fall Risk Assessment: For an elderly patient at risk of falling, the nurse assesses gait, balance, mobility, and factors contributing to the fall risk.
- Nutritional Assessment: On a malnourished patient, the nurse assesses dietary intake, weight changes, body mass index, and signs of malnutrition.
- Skin Assessment: For a patient with pressure ulcers, the nurse assesses skin integrity, identifies pressure points, and evaluates the wound’s healing progress.
What are Nursing Assessment Tools?
Nursing assessment tools are instruments or frameworks that assist nurses in systematically collecting and documenting patient data.
Here’s a list of commonly used nursing assessment tools:
- Glasgow Coma Scale (GCS): Assesses a patient’s level of consciousness, eye-opening response, verbal response, and motor response.
- Pain Assessment Scales: Examples include the Visual Analog Scale (VAS), Numeric Rating Scale (NRS), and Faces Pain Scale, used to assess the intensity of a patient’s pain.
- Bradford Hill Criteria: Used in epidemiology, this tool helps evaluate the strength of association between exposure to a factor and the occurrence of a disease.
- Mini-Mental State Examination (MMSE): Assesses cognitive function and detects cognitive impairment, commonly used in assessing dementia.
- Nutritional Assessment Tools: These include the Mini Nutritional Assessment (MNA) and Malnutrition Universal Screening Tool (MUST), which evaluate a patient’s nutritional status.
- Norton Scale: Assesses the risk of developing pressure ulcers based on factors like physical condition, mental state, activity level, mobility, and incontinence.
- Falls Risk Assessment Tools: Examples include the Morse Fall Scale and Hendrich II Fall Risk Model, used to identify patients at risk of falling.
- Edmonton Symptom Assessment System (ESAS): Used to assess and manage multiple symptoms in patients with cancer or other illnesses.
- Modified Early Warning Score (MEWS): Evaluates vital signs to identify deteriorating patients early, preventing adverse outcomes.
- Beck Depression Inventory (BDI): A self-report questionnaire used to assess the severity of depression symptoms.
- Bristol Stool Form Scale: Assesses the consistency of feces to evaluate gastrointestinal health.
- CAGE Questionnaire: Screens for alcoholism by asking about feeling the need to cut down, annoyance by criticism, guilt about drinking, and eye-openers.
- Confusion Assessment Method (CAM): Used to detect delirium in patients, particularly those with altered mental status.
- Functional Independence Measure (FIM): Evaluates a patient’s level of disability and required assistance in performing daily activities.
- Modified Barthel Index: Assesses a patient’s ability to perform activities of daily living, providing insight into their level of independence.
- Palliative Performance Scale (PPS): Measures the functional status of patients with advanced illness, assisting in care planning.
- Perinatal Depression Screen: Various tools, like the Edinburgh Postnatal Depression Scale (EPDS), assess maternal mental health during pregnancy and postpartum.
What is ABC in Nursing?
In nursing, “ABC” stands for Airway, Breathing, and Circulation.
It represents a priority framework used to quickly assess and prioritize patient care in emergency situations, especially those involving potential life-threatening conditions.
- Airway: This refers to assessing the patency (openness) of the patient’s airway. If the airway is blocked or compromised, it must be cleared to allow the patient to breathe.
- Breathing: The assessment of the patient’s breathing involves evaluating their respiratory rate, effort, and the presence of any distress. Addressing breathing issues promptly is crucial for maintaining oxygenation.
- Circulation: This focuses on evaluating the patient’s circulation, including heart rate, blood pressure, and overall perfusion. Ensuring proper circulation is essential for delivering oxygen and nutrients to the body’s tissues.
The ABC approach is a fundamental principle in healthcare, especially in critical care settings and during resuscitation efforts.
It helps healthcare professionals quickly identify and address the most critical issues to stabilize the patient’s condition and prevent further deterioration.
Conclusion
Nursing assessment, in essence, establishes a fundamental and comprehensive understanding of the patient’s health status, preferences, and contextual factors.
This fundamental knowledge serves as a foundation for developing individualized care plans, making sound clinical decisions, and facilitating effective communication among members of the healthcare team.
Recommended Readings
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Kozier & Erb’s Fundamentals of Nursing: Concepts, Process and Practice, 11th edition


Comments are closed.