Last updated on December 28th, 2023
In this article, you will learn about the anatomy and physiology of the integumentary system along with their main functions. As well as accessory structures of the skin and their function.
Anatomy & Physiology of The Integumentary System
The integumentary system is composed of skin and its associated structures. It is the outermost layer of the body containing skins and appendages.
Appendages refer to the accessory structures like hair, nails, and glands. Other associated structures include blood vessels, nerves, and sensory organs.
The main organs in the integumentary system are skin, hair, nail, and glands.
The integumentary system is the largest body system and works to protect and maintain the internal environment.
The skin layers and their function
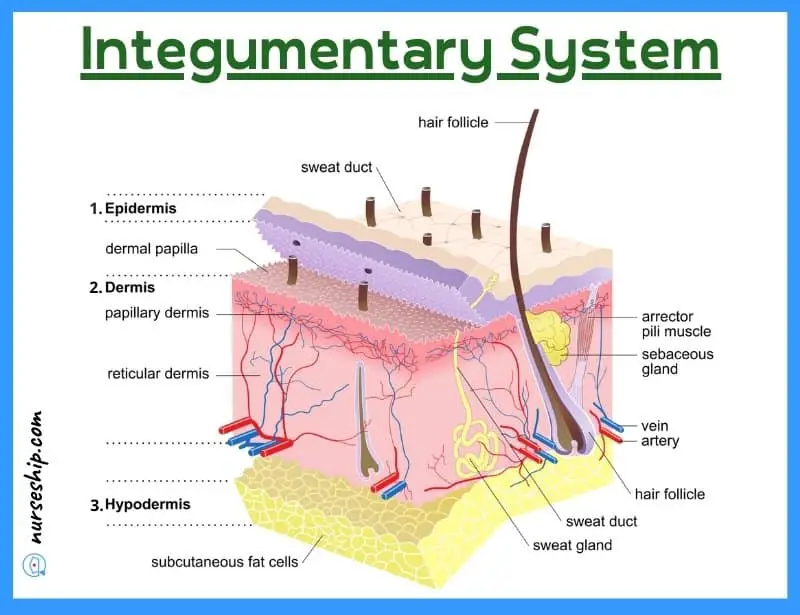
The skin is comprised of three layers, which are:
- Epidermis
- Dermis
- Hypodermis
1. Epidermis
The epidermal layer of the skin is the outermost superficial layer ranging in thickness from 0.1mm to 1 mm depending on the different regions. It is thickest on the palms and soles.
The epidermis is avascular and is mainly comprised of flattened and keratinized squamous epithelial cells. It derives its nutrition from the underlying vascular dermis.
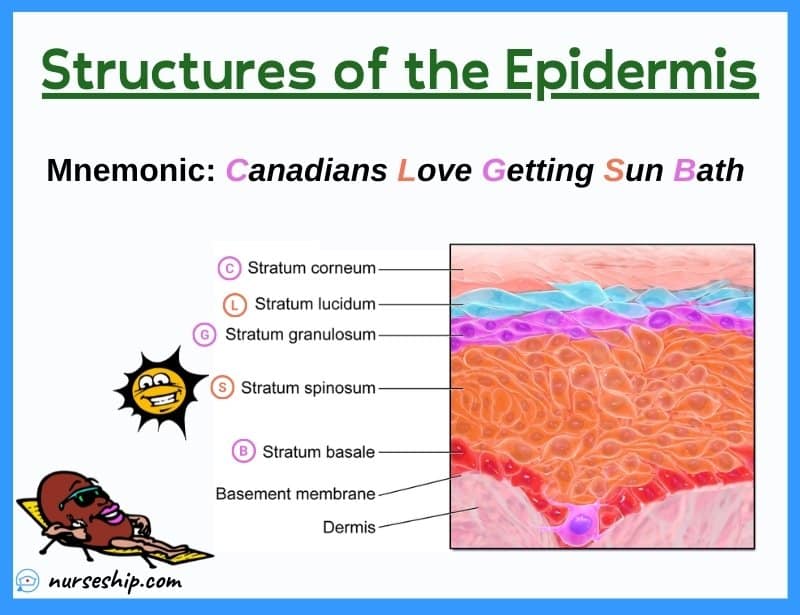
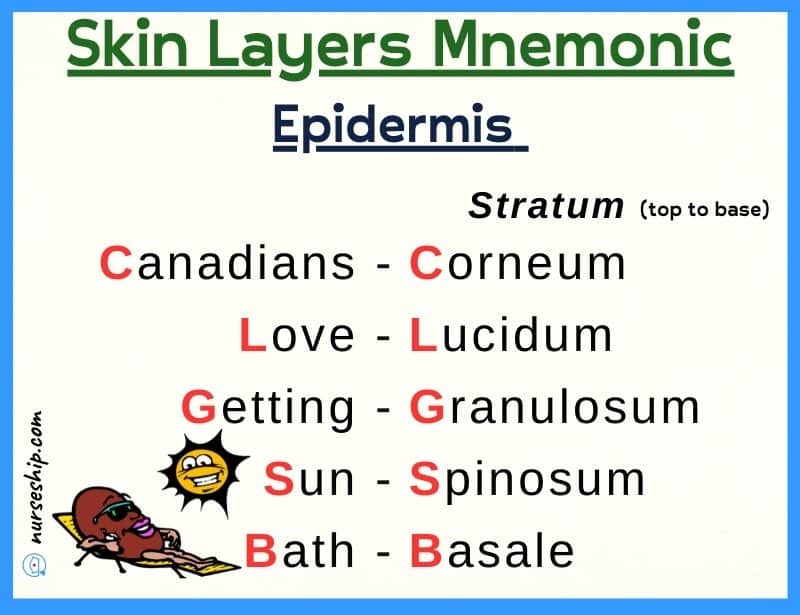
The epidermis is further divided into 3 to 5 layers:
- Stratum Corneum: It is the topmost keratinized layer that sheds the dead cells continuously to replace them with newly formed keratinocytes from the layers beneath it. It mainly has up to 30 layers of dead and flat keratin-coated cells which makes it durable and resistant.
- Stratum Lucidum: This is also known as the clear layers and is absent in most regions. When present, it prevents the loss of water from the skin.
- Stratum Granulosum: This granular layer plays its role in the synthesis of keratin which is a resistant protein made by the fibroblast cells.
- Stratum Spinosum: As the name suggests, it is the spiny layer that is rich in RNA (Ribonucleic acid) and plays an important role in the keratinization of cells.
- Stratum Basale: Stratum Basale is also known as stratum germinativum or the stem cell layer. Composed mainly of columnar cells, it is where the new cells are continuously synthesized and moved towards the stratum corneum.
As the cells continue to travel towards the top, they began to lose their cytoplasm and nucleic acid which is replaced by keratin formation within the cells. Therefore, they become thickened and flattened before reaching the top layer where they replace the exfoliated cells.
The deeper layers of the epidermis also contain specialized cells called melanocytes that produce melanin pigment. This pigment is responsible for skin tone.
2. Dermis
The dermis is the inner vascular layer of the skin which is mainly composed of connective tissue, fibers, glands, nerve endings, and hair follicles.
The dermis is further divided into two zones:
- Papillary layer
- Reticular layer
The papillary layer of the dermis is composed of finger-like projections that interdigitate with the epidermal layer. These finger-like projections are unique to every individual and are responsible for distinct fingerprints.
The reticular layer is composed of fibers and appendages.
The following types of fibers are found in the extracellular matrix of the dermis:
– Collagen fibers: Mainly responsible for resistance and strength.
– Elastic fibers: Provides elasticity to the skin.
In addition to this, the dermis has a rich vascular supply, sebaceous and sweat glands, and hair follicles. Most of the important functions of the skin are therefore carried out by the dermis.
3. Hypodermis
It is present beneath the dermis and is also known as the subcutaneous layer. It is composed of blood vessels, nerves, and adipose cells. These adipose cells are filled with fat.
The function of subcutaneous tissue is mainly:
- Insulation
- Storage of energy
- Shock absorption
Because of its vascularity, certain medications like insulin are specifically injected into this layer.
Human Anatomy & Physiology Course
- Guidebooks
- Complete Diagrams & Lessons
- Certifications
- Quiz & Answers
- And More…
Functions of the integumentary system
The integumentary system serves several important functions in the human body. The following are five important functions of the integumentary system.
1. Thermoregulation
Thermoregulation literally means regulation of the body temperature. Maintaining an optimum body temperature is imperative to the smooth functioning of the body systems. Hence, making it one of the most important functions of the skin.
Temperature is controlled by changing the diameter of the lumen of blood vessels and thus increasing or decreasing the surface blood supply.
Exposure to a cold external environment constricts blood vessels and decreases blood flow to the surface to conserve body heat.
In contrast, the blood vessels dilate on exposure to hot external environments. The dilation increases the blood flow to the surface to overheating of the body.
2. Protection against infection
The skin forms a barrier between the external and internal environments and protects against invading pathogens. It does so by:
- maintaining surface integrity by tight intracellular contacts.
- constant shedding and migration of the cells help in manually decreasing the surface pathogens. It can also help in repairing and maintaining a high turnover.
Any break in the barrier due to wounds or injuries can lead to infections.
3. Barrier against dehydration
The skin not only acts as a barrier against the invading pathogens but also against the unwanted loss of water from the skin.
Special sebum-producing glands called sebaceous glands help in producing an overall layer of a waterproof surface barrier.
Keratin in the superficial layer also helps in the conservation of water to prevent dehydration.
Notably, this barrier is lost in burn patients leading to significant fluid loss.
4. Vitamin D synthesis
Vitamin D is essential for healthy bone growth. The epidermal layer of skin synthesizes vitamin D upon exposure to UV radiations or sunlight. Vitamin D3 (Cholecalciferol) is synthesized from cholesterol derivatives.
The liver and kidneys then work to convert it into its active form.
Vitamin D plays a significant role in the absorption of calcium and phosphorous.
Lack of D3 can lead to weaker bones or even Rickets in children and Osteomalacia in adults.
5. Sensory perception
A key function of the skin is sensory perception. It has many sensory nerve endings and receptors that can detect the sensations of hot, cold, touch, pressure, and pain.
Additionally, Autonomic nerve fibers are present that carry impulses to the smooth muscles n Blood vessels, hair roots, and sweat glands.
Accessory structures of the skin and their functions
The accessory structures of the skin are the appendages and it includes:
- Hair
- Nails
- Glands: Sebaceous and sweat glands
Let’s briefly discuss each skin’s accessory structures and their functions:
Accessory structures of the skin: The hair
The human body is covered with hair. Except for a few regions like palms, soles, lips, nipples, and certain parts of genital regions.
The hair serves many important insulating and protective functions that will be discussed later.
Hair structure has three main parts:
- Shaft
- Follicle
- Hair bulb
Shaft
The hair shaft is the part of the hair that projects above the skin and is visible to the naked eye.
Hair follicle
The hair follicle lies in a sheath of epithelial cells. It has a rich blood and nerve supply.
A thin band of muscles called arrector pili is attached to the hair follicles. This muscle is responsible for the goosebumps that occur due to the erection of hair standing upon being frightened or when exposed to cold.
Additionally, melanocytes are present here that produces pigments responsible for different hair colors.
Hair bulb
The hair bulb or root is buried in the dermis. It is the lowest part of the hair where growth occurs.
Surrounding it is a cluster of blood vessels and capillaries which make up the hair papillae and is responsible for providing nourishment.
New hair growth also occurs by the stem cells present in this region.
Function of hair
The hair serves the following important functions:
1. Temperature regulation:
Hair in mammals helps in keeping the body temperature stable.
2. Extends the sense of touch:
The sense of touch is extended by hair. An example of this is that we can detect something even before it touches the skin. A study was published in 2012 by John Hopkins university regarding this.
3. Protective functions:
The hair also serves to protect the body against harmful particles. For example, the eyelids and nasal hair are protective.
4. Identification:
It is one of the least discussed aspects but hair plays a vital role in identifications during forensic studies.
Accessory structures of the skin: The nail
The nails are present on the end of fingers and toes on their distal surface. These are composed of densely keratinized epithelium.
It has the following parts:
1. Nail plate:
The visible part of the nail is called the nail bed. It has a free edge and a proximal edge attached to the nail root.
2. Nail bed:
The nail bed is a layer of epithelium on which the nail plate rests.
Its rich blood supply results in a pinkish appearance of the nails.
3. Lunula:
It is the crescent-shaped white area at the base of the nail
4. Cuticle:
It is the skin fold that surrounds the nail body. The cuticle is an extension of the stratum corneum.
5. Nail root:
The nail root is the proximal end of the nail. It is where the new keratinized cells are added by the underlying nail matrix.
An average fingernail grows by 1mm each week. The growth is however slower in toenails.

Function of nail
Functions of the nail include:
- Protection of fingers and toes
- Scratching
- Manipulation of small objects
- Improves grip
Accessory structures of the skin: The glands
The glands are specific organs that produce or release substances necessary for various body functions.
Three types of glands are mainly present in the skin.
- Sweat glands
- Sebaceous glands
- Ceruminous glands
1. Sweat Glands
There are primarily two types of sweat glands or sudoriferous glands:
i. Eccrine glands
These types of sweat glands are distributed throughout the body with a few exceptions like lips or glans penis.
These glands have a coiled tube-like structure that produces secretions that are directly released on the skin surface by its excretory duct.
The secretion is named sweat which contains water and salts. Notably, the sodium concentration in sweat is similar to that of plasma.
On average, 500ml of sweat is secreted in one day. It can increase with exertion and decrease in cold weather conditions.
- The main function of sweat is the maintenance of core body temperature
- Since sodium, potassium, lactic acid, and uric acid are also secreted in sweat, it also helps in eliminating waste.
ii. Apocrine glands
The Apocrine glands do not release their secretions directly on the skin surface. Rather they do so at the base of hair follicles.
These types of sweat glands are present in the axillae (armpit) and groin regions and start functioning after puberty.
It is released in response to fear or sexual stimulation. The sweat itself is colorless and odorless but contains some cellular material that is broken down by bacteria after accumulation on the skin.
The by-products of this breakdown result in the typical odor of sweat.
They do not have any specific function.
2. Sebaceous glands
The sebaceous glands are associated with the hair follicles and produce a special secretion called sebum. This sebum combines with sweat and forms an oily layer that protects the hair and skin.
It not only prevents dryness but also has slight anti-bacterial and anti-fungal properties.
Sebaceous glands can be found in every region except the palms and soles.
Modified sebaceous glands named meibomian glands are present in eyelids and protect the eyes against dryness and lubricate them.
Sebum can also accumulate over time and can lead to clogged ducts leading to pimples and blackheads.
3. Ceruminous Glands
These glands are mainly present on the surface of the ear canal and produce ear wax. Ear wax is also known as cerumen. This keeps our ear canal moist.
However, excessive wax accumulation can lead to ear infections and hearing loss.
Conclusion
The integumentary system along with the accessory structures of the skin performs a wide range of functions that are essential to a person’s overall health and well-being.
References
Lippincott Williams & Wilkins. (2009). Anatomy and physiology made incredibly easy! (3rd ed.).
Cohen, B., & Taylor, J. (2009). Memmler’s Structure and Function of the Human Body, 8th ed (10th ed.). Lippincott Williams & Wilkins.
Thompson, G. (2015). Understanding Anatomy & Physiology: A visual, auditory, interactive approach (2nd ed.). F. A. Davis Company.