In this post, you will find 25 NANDA nursing diagnosis for Breast Cancer. These include actual and risk nursing diagnoses.
Breast cancer nursing assessment, interventions, priorities, and patient teaching are all included.
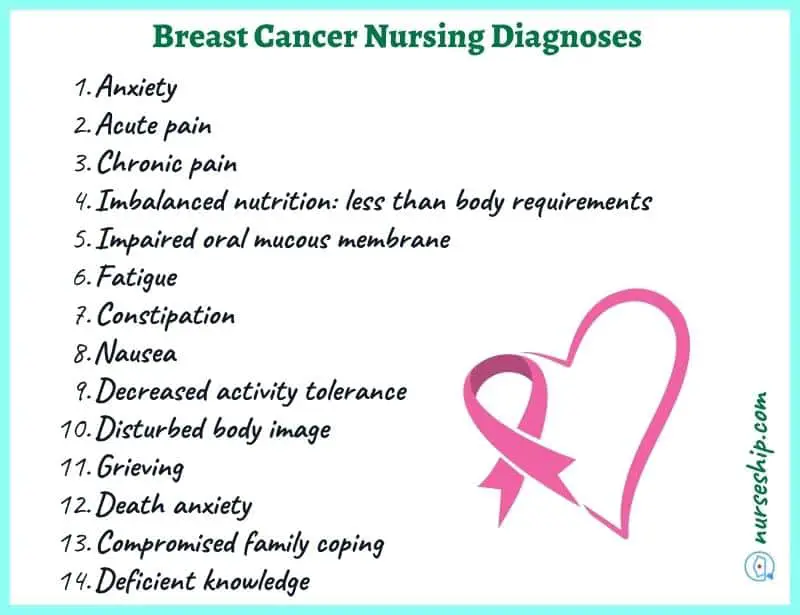
25 NANDA nursing diagnosis for Breast Cancer
- Anxiety
- Acute pain
- Chronic pain
- Imbalanced nutrition: less than body requirements
- Impaired oral mucous membrane
- Fatigue
- Constipation
- Nausea
- Decreased activity tolerance
- Disturbed body image
- Grieving
- Death anxiety
- Compromised family coping
- Deficient knowledge
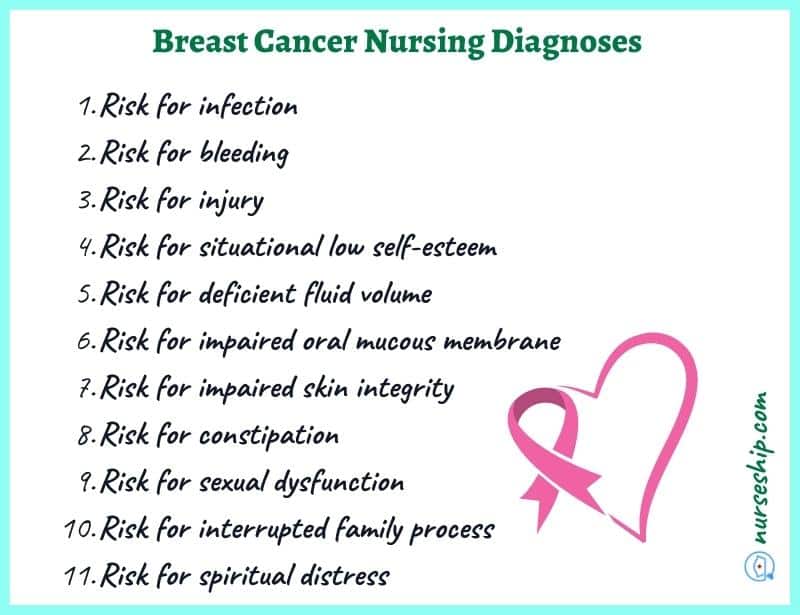
- Risk for infection
- Risk for bleeding
- Risk for injury
- Risk for situational low self-esteem
- Risk for deficient fluid volume
- Risk for impaired oral mucous membrane
- Risk for impaired skin integrity
- Risk for constipation
- Risk for sexual dysfunction
- Risk for interrupted family process
- Risk for spiritual distress
NANDA nursing diagnosis for Breast Cancer
#1 Anxiety
| May be related to | As evidenced by |
| Fear of treatment therapy and treatment related side effects, threat of death, major life change (economic, health and role function implications), anticipated body changes, separation from support system | Decreased tolerance to pain, insomnia, nausea and vomiting, distress, hypertension, tachycardia, increase in tension, apprehensiveness, feeling of inadequacy, restlessness |
#2 Acute pain
| May be related to | As evidenced by |
| Nerve tissue compression, nerve tissue destruction, inflammation process, chemical agents e.g. chemotherapy and radiotherapy, neoplasms | Verbal reports of severe pain, facial mask, changes in vital signs, restlessness, irritability, inability to perform activities of daily living (ADLs), lack of appetite, positioning to promote comfort, altered sleep pattern |
#3 Chronic pain
| May be related to | As evidenced by |
| Post chemotherapy pain syndrome (chemotherapy-induced peripheral neuropathy, stomatitis/mucositis) post radiation pain syndrome (skin burns, mucositis, scarring), infiltration into nerves, metastatic bone pain, post-surgical pain, phantom pain | Facial mask, self-restriction to one position, depression, verbal reports of persistent pain, anorexia, expression of fatigue, reports of pain intensity and characteristic, altered sleep-wake cycle |
#4 Imbalanced nutrition: less than body requirements
| May be related to | As evidenced by |
| Anorexia, nausea, loss of appetite, fatigue, hyper metabolic state, gastric irritation, depression, inability to ingest food, insufficient intake, altered taste perception, food aversion, sore buccal cavity | Recent weight loss, wasted muscle mass, electrolyte imbalance, hypoglycemia, abdominal cramping, decreased food intake, lack of interest in food, halitosis, sore buccal cavity, constipation, abdominal pain |
#5 Impaired oral mucous membrane
| May be related to | As evidenced by |
| Ineffective oral hygiene, chemotherapy related side effects, poor nutritional status, presence of gingival infection, metastatic oral cavity/neck lesions | Dry tongue, cracked lips, lesions in buccal cavity, xerostomia, buccal pain and discomfort, reluctance to feed |
#6 Fatigue
| May be related to | As evidenced by |
| Side effects of treatment therapy: chemotherapy, biotherapy or radiation induced, anemia, anxiety and depression, malnutrition | Lack of energy, lethargy, inability to perfume activities of daily living independently, reduced concentration, lack of interest in surrounding, social withdrawal, feelings of hopelessness/helplessness |
#7 Constipation
| May be related to | As evidenced by |
| Chemotherapy treatment, use of opioids, changes in diet, insufficient consumption of fluids, lack of activity/immobility, altered regular routine, impaired physical mobility | Less than 3 bowel movements in a week, abdominal distention, blood in stool, hard lumpy stool, straining to pass faces, feeling of insufficient bowel emptying after defecation, sensation of anorectal obstruction |
#8 Nausea
| May be related to | As evidenced by |
| Chemotherapy, radiation therapy, anxiety, fear, noxious taste | Refusal to feed, food intolerance, hyper salivation, retching, vomiting, uneasiness in the back of the throat, chest and abdomen, diaphoresis, increased swallowing |
#9 Decreased activity tolerance
| May be related to | As evidenced by |
| Poor perfusion secondary to anemia induced by chemotherapy drugs or radiation therapy, comorbidities such as renal failure, surgery related restrictions, pain syndromes, decreased muscle mass, malnutrition, impaired physical mobility | Verbal reports of fatigue, exertional dyspnea, dizziness, headaches, fainting spells, tachycardia with diminished peripheral pulse, generalized weakness, diaphoresis, cyanosis, anxiety when needed to perform ADLs |
#10 Disturbed body image
| May be related to | As evidenced by |
| Alopecia, severe weight loss/cachexia, sterility, persistent pain, impotence/sterility, chemotherapy or radiation induced nausea and vomiting, mastectomy, death threat, helplessness, doubts concerning acceptance by significant other, overwhelming fatigue | Preoccupation with body changes/loss of body part(breast), negative feelings about self, feelings of powerlessness and helplessness, lack of follow through with instructions, self-neglect (failure to perform self-care), fear of rejection |
#11 Grieving
| May be related to | As evidenced by |
| Anticipated loss of social status, economic stability, home, family or significant other, body function or body part, death threat | Reduced tolerance to pain, self-blame or shifting blame on other people/objects, altered sleep pattern, social withdrawal, anxiety and depression, decreased activity level, hopelessness |
#12 Death anxiety
| May be related to | As evidenced by |
| Facing the reality of terminal illness, perceived impending death, uncertainty of continuity of life after physical death, anticipation of family grief on death | Fear of dying and suffering/pain related to dying, anger, shifting blame on other people/events, despair, psychological distress, preoccupation with death, |
#13 Compromised family coping
| May be related to | As evidenced by |
| Insufficient support, disorganization, lack of understanding of diagnosis/family role, comprehensive treatment therapy | Hostility to healthcare staff, limited communication between client and caregiver, client concern on caregiver/family response to diagnosis, protective behavior by caregiver without regard to client’s autonomy, family withdrawal of support for client |
#14 Deficient knowledge
| May be related to | As evidenced by |
| Unfamiliar disease process, complex treatment options (chemotherapy, radiation therapy, immunotherapy among others), unfamiliar environment | Verbal expressions of misconception/ inaccurate information, questing healthcare team, hesitance to make decisions, hostility towards healthcare teams, lack of follow through with instructions |
Risk nursing diagnosis for Breast Cancer
#1 Risk for infection
Associated risk factors
- Compromised skin integrity
- Immunosuppression
- Malnutrition
- Invasive procedures and devices
#2 Risk of situational low self-esteem
Associated risk factors
- Debilitating illness
- Functional impairment
- Lack of control
- Altered body image
#3 Risk for deficient fluid volume
Associated risk factors
- Fluid loss via normal routes: diaphoresis, vomiting and diarrhea
- Fluid loss via abnormal routes: wounds, indwelling tunes
- Lack of oral intake
- Malnutrition
- Hyper-metabolic state
- Insufficient muscle mass
#4 Risk for impaired oral mucous membrane
Associated risk factors
- Side effects of treatment therapy: chemotherapy, radiation therapy
- Nil by mouth status for long periods
- Dehydration
- Malnutrition
#5 Risk for impaired skin integrity
Associated risk factors
- Poor nutritional status
- Immobility
- Effects of chemotherapy
- Radiation
- Immunocompromised status
#6 Risk for constipation
Associated risk factors
- Lack of sufficient fiber in meals
- Insufficient fluid intake
- Malabsorption syndrome
- Gastrointestinal inflammation
- Use of opioids
- Radiation therapy
#7 Risk for sexual dysfunction
Associated risk factors
- Alternation in body function
- Changes in physical body structure
- Psychological side effects of terminal disease
- Specific sexual difficulties such as vaginal dryness
- Lack of privacy
#8 Risk for interrupted family process
Associated risk factors
- Poor prognosis
- Shift in family roles
- Financial difficulties
- Changes in health status of a family member
- Situational crises
#9 Risk for spiritual distress
Associated risk factors
- Anticipation of impending death
- Low self-esteem
- Anxiety and depression
#10 Risk for bleeding
Associated risk factors
- Thrombocytopenia associated with chemotherapy and radiotherapy
#11 Risk for injury
Associated risk factors
- Improper disposal of chemotherapeutic agents
- Confusion (late-stage cancer)
- General body weakness
Nursing Priorities for Breast Cancer
- Support adaptation and independence
- Promote comfort through adequate pain management
- Patient safety
- Maintain optimal physiological functioning
- Prevention and management of complications
- Monitoring for and prevention of disease advancement
- Maintaining the quality of life
- Provide information about the disease process, condition, prognosis, and treatment needs.
Nursing management for Breast Cancer
Nursing Assessment
- Assess and monitor vital signs
- Assess the patient’s comprehensive history, noting the family history of cancer, age at menarche, first child’s birth, number of children, and menopause.
- Note the characteristics of the breast mass such as primary site, initial date of discovery/diagnosis, and additional sites involved (metastasis)
- Assess for changes in auxiliary or supraclavicular lymph nodes
- Assess the patient’s health maintenance habits such as knowledge and practice of breast self-exam (BSE), history of mammograms, diet habits to including intake of alcohol and fats, and use of hormone supplements.
- Perform a physical exam: note the shape and size of the breast, fixation to bordering tissues, skin changes, presence of discharge (and characteristics if present), and pain
- Explore the patient’s level of education and readiness to learn to establish a teaching plan.
| Subjective data | Objective data |
| Breast size/shape change | Inverted nipple |
| Localized pain | Hard, irregular lumps and immobile lumps |
| Nipple inversion | Changes in breast contour |
| Skin dimpling on the affected breast | Wasting of muscle mass |
| Lump(s) at the axillary region | Edema and pitting |
| Nipple discharge (blood-stained) | Ulcerated oral mucosa |
| Skin change on the affected breast | Peau d’orange |
| Recent weight loss | Hypertension and tachycardia |
| Fatigue and weakness | Compromised concentration |
| Denial of diagnosis | Facial mask of pain and discomfort |
| Hopelessness and helplessness | Depression/social withdrawal |
| Poor dietary habits | Severe weight loss/cachexia |
| Nausea and vomiting | Poor skin turgor |
| Changes in bowel pattern | Diminished bowel sounds |
Nursing Interventions
- Review the client’s and significant other’s (SO) prior cancer treatment experience. Find out what the doctor informed the patient and what conclusion the patient came to. Encourage the customer to express their feelings.
- Create a relaxed atmosphere where clients can express their emotions or choose not to speak at all.
- Keep in close communication with the client. As necessary to build trust, speak with and touch the client.
- Help the client and family identify their anxieties and clarify them so they may start to create coping mechanisms.
- Give reliable, consistent information on the diagnosis and outlook. Avoid arguing about how the client sees the problem.
- Provide non-pharmacologic pain management measures such as massage, repositioning, music, TV, and other diversion measures.
- Inform the patient, and monitor side-effects of chemotherapy and radiation such as alopecia, nausea and vomiting, weight changes, xerostomia, sore throat, bone marrow suppression, anxiety, and depression
- Monitor the client’s daily food consumption and ask them to keep a food diary as directed.
- Encourage the customer to have a high-calorie, nutrient-rich diet while also getting enough fluids. Offer wholesome nourishment and encourage the consumption of supplements and frequently spaced, smaller meals.
- Support and address the patient psychological needs throughout, from diagnosis to treatment.
- Explain pre-, intra-, and post-op phases of surgical procedures to alleviate anxiety and fear
- Anticipate alopecia and fatigue post-chemo and plan with the patient appropriately.
- Involve the patient in the planning and execution of treatment
- Administer antiemetic prophylaxis for chemo patients as indicated
- Administer intravenous infusion, antianxiety medication, and analgesics as indicated
- Help the patient to find an accountability partner from their family/friends circle/community
- Suggest measures to deal with/address anxiety, depression, and sexual dysfunction such as understanding the treatment process, having support persons
Patient teaching for Breast Cancer
- Minimize uncertainty by correcting/clarifying misinformation
- Explain the treatment options
- Provide information on post-mastectomy care
- Develop realistic expectations of the treatment as per cancer staging
- Set realistic goals with patient
- Establish support networks such as support groups, accountability partners
- Explore information sources
- Encourage exploration of spirituality/faith
- Instruct on how to use patient-controlled analgesics
- Involve family in decision-making and health education sessions
- Encourage regular follow-up, screenings, diet modifications, and exercise (early stages)
- Teach stress reduction techniques
Conclusion
To sum up, you now know 25 NANDA nursing diagnosis for Breast Cancer that you can use in your nursing care plans.
Additionally, you have also learned about nursing assessment, nursing interventions, nursing priorities, and patient teaching for Breast Cancer.
Reference
Ackley, B., Ladwig, G., Makic, M., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing Diagnoses Handbook: An Evidence-based Guide to Planning Care (12th ed.). Elsevier.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2013) Nurses pocket guide: Diagnoses, interventions, and rationales (13th ed.). F. A. Davis Company
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, and outcomes. Elsevier Health Sciences.
Herdman, T., Kamitsuru, S. & Lopes, C. (2021). NURSING DIAGNOSES: Definitions and Classifications 2021-2023 (12th ed.). Thieme.
Swearingen, P. (2016). ALL-IN-ONE Nursing Care Planning Resource (4th ed.). Elsevier/Mosby.